Benign Paroxysmal Positional Vertigo - BPPV
Reading time: 5 minutes
Benign paroxysmal positional vertigo (BPPV) is the most common cause of dizziness and vertigo. (1-4) The condition is characterized by brief episodes of dizziness, nausea, or nystagmus triggered by head movement. (5) Over seven percent of the population will experience BPPV at some point in their lifetime, and 80% of those patients will require medical treatment. (6,7)
An October 2022 systematic review in Academic Emergency Medicine concluded that canalith repositioning maneuvers (aka Epley maneuver) should be the first line of care for BPPV:
In patients with BPPV, vestibular suppressants may have no effect on symptom resolution at the point of longest follow-up; however, there is evidence toward the superiority of CRM over these medications. Vestibular suppressants have an uncertain effect on symptom resolution within 24 h, repeat ED/clinic visits, patient satisfaction, quality of life, and adverse events. These data suggest that a CRM, and not vestibular suppressants, should be the primary treatment for BPPV. (104)
This conclusion means manual therapists should be the provider of choice for BPPV patients. So, to make sure you own the essential skills, check out this BPPV - Benign Paroxysmal Positional Vertigo Epley maneuver video, including the pre-requisite Dix-Hallpike test.
Want a refresher for your treatment room?
Subscribers can download the following Epley maneuver PDF in the forms library. Not a subscriber? Fill out the form below to receive your download in your inbox!
*The remainder of this blog has been optimized as an interactive experience for ChiroUp subscribers logged in to their accounts.
BPPV Symptoms
The classic presentation for BPPV includes sudden (aka paroxysmal) episodes of rotary vertigo that last 10-20 seconds following head position changes. (5,36) Typical provocative activities involve transitioning between upright and recumbent positions; rolling from side to side in bed; bending forward; and moving the head to look up, down, or side to side. (37)
BPPV Exam
The BPPV exam's primary purpose is to rule out more sinister causes of vertigo and to identify the side (right, left, both) and site (posterior, anterior, horizontal) of the involved semicircular canal. Clinicians should remember that multiple canals can be involved (4.6% of cases), and the condition can be bilateral. (39,97)
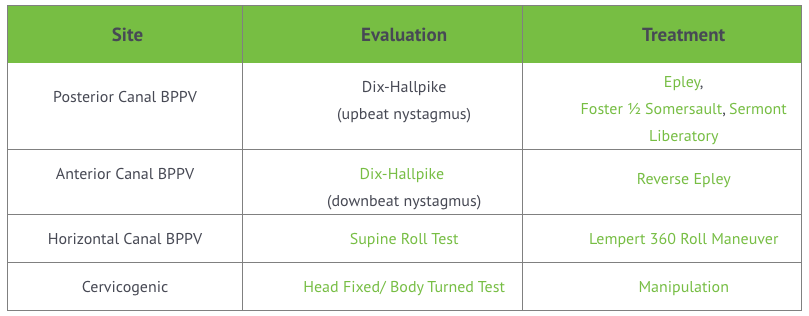
BPPV can arise from any semicircular canal (posterior, anterior, and horizontal). The following chart outlines evaluation and management options for each.
The Most Versatile BPPV Test
Most cases of BPPV (60-90%) involve the posterior semicircular canal. (7,40,41) The Dix-Hallpike maneuver is the gold standard BPPV test for diagnosing posterior canal BPPV. (42-44,50) The Dix-Hallpike test has a specificity of 83% and a sensitivity of 52% for posterior canal BPPV. (46,47) ChiroUp subscribers can review the Dix-Hallpike test here.
The Difference Between BPPV and Cervical Vertigo
Cervicogenic vertigo (arising from irritated neck joints) presents with symptoms similar to BPPV, i.e., episodic, provoked by movement, and eased by maintaining a stable position. Patients may complain of light-headedness, floating, unsteadiness, or general imbalance, but rarely true “spinning” vertigo (84). Cervicogenic vertigo is often accompanied by loss of cervical range of motion, upper cervical tenderness, and upper cervical segmental joint restriction. (85,86)
One complicating factor for differentiating cervicogenic vertigo from BPPV is that most provocative movements simultaneously stimulate cervical spine proprioceptors and the vestibular apparatus.
The Head-fixed/body-turn test (aka Neck torsion test) aims to isolate cervical mechanoreceptors without stimulating the vestibular apparatus. (87,88) The neck torsion test is performed with the patient rotating their body on an exam stool while the clinician stabilizes their head, thereby minimizing vestibular input. Reproduction of dizziness or nystagmus when the head is stable suggests a cervical component. (89-91) Subscribers can review the Head-fixed/body-turn test here.
BPPV Treatment
Canalith repositioning maneuvers and BPPV home exercises are the current standard of care for the treatment of BPPV. (40,42,43,47-49) BPPV treatments are predicated upon identifying the involved semicircular canal(s) and then choosing the appropriate maneuver to reposition the wayward calcium carbonate sediment. (2,37) All BPPV repositioning maneuvers attempt to move the head into a position where debris can fall to the top of the problematic canal and then transition the head into a position where the debris moves around the canal back into the vestibule.
The Epley Maneuver
When the posterior semicircular canal is involved, clinicians should choose the canalith repositioning procedure, aka, Epley maneuver for vertigo. (42-44) The effectiveness of the Epley maneuver ranges between 78-95%. (62) A single Epley BPPV maneuver leads to remission in 44-89% of cases, and this rate improves with second, third, or fourth interventions. (2) The addition of vibration does not enhance the effectiveness of the Epley canalith repositioning maneuver for BPPV. (64,65)
ChiroUp subscribers can review the benign paroxysmal positional vertigo Epley maneuver video below, aka, canalith repositioning procedure video.
Pro tips: When performing repositioning maneuvers, movement should be brisk enough to generate sufficient momentum to dislodge displaced canaliths. Clinicians should also recognize these crystals are moving through fluid, which requires an adequate amount of time to settle into a new position. Clinicians should proactively inform patients that although they may become dizzy during testing or treatment, they should attempt to keep their eyes open and remember the intervention will ultimately help ease their symptoms.
Subscribers can review the ChiroUp BPPV protocol for a complete description, including contraindications to performing the Epley maneuver. (i.e., instability, recent cervical spine surgery, vascular issues, detached retina, or advanced arthritis) (73,74)
BPPV Outcomes
Did you know that the ChiroUp Clinical Outcomes & Patient Satisfaction Synopsis found BPPV was the most responsive condition of all 115 ChiroUp diagnoses?
At-Home BPPV Exercises
Home exercises for BPPV can provide supportive benefits. Exercises for posterior canal BPPV include the Foster half somersault and the Sermont liberatory maneuvers. Subscribers can review those here.
Need a BPPV patient handout, including the best exercises for BPPV? ChiroUp has you covered.
In less than 4 clicks subscribers can share fully customizable condition reports with your patients in seconds.
✔ Condition-specific exercises & recommendations
✔ Customizable to your care
✔ Branded to your clinic
✔ Multilingual options
Want more BPPV content?
Join our docs for an entertaining and informative discussion about the most common causes of vertigo. This on-demand webinar will include practical skills for managing cervicogenic vertigo and BPPV, plus valuable tips for identifying threatening presentations.
-
1. Teixido M, Woods O, Kung B, Seyyedi M. A 3D benign paroxysmal positional vertigo model for study of otolith disease. World journal of otorhinolaryngology-head and neck surgery. 2016 Mar 1;2(1):1-6. Link
2. Fife TD, von Brevern M. Benign paroxysmal positional vertigo in the acute care setting. Neurologic clinics. 2015 Aug 1;33(3):601-17. Link
3. Brandt T. Vertigo: its multisensory syndromes. London: Springer; 1999. 503p.
4. Haybach PJ, Underwood JL. BPPV: what you need to know. Vestibular Disorders Association; 2000.
5. Caldas MA, Ganança CF, Ganança FF, Ganança MM, Caovilla HH. Clinical features of benign paroxysmal positional vertigo. Brazilian journal of otorhinolaryngology. 2009 Aug;75(4):502-6. Link
7. Caldas MA, Ganança CF, Ganança FF, Ganança MM, Caovilla HH. Clinical features of benign paroxysmal positional vertigo. Brazilian journal of otorhinolaryngology. 2009 Aug;75(4):502-6. Link
8. S. Ritchie, J. Corcoran, M. Liston, G. Jones. The Prevalence of Benign Paroxysmal Positional Vertigo (BPPV) in an Outpatient Physiotherapy Setting for Older Adults. Physiotherapy 2015; Volume 101, Supplement 1 eS1238–eS1642
9. Baloh RW, Honrubia V, Jacobson K. Benign positional vertigo: clinical and oculographic features in 240 cases. Neurology. 1987 Mar 1;37(3):371-. Link
10. Herdman SJ, Tusa RJ. Avaliação e tratamento dos pacientes com vertigem posicional paroxística benigna. Reabilitação Vestibular, 2ª ed., São Paulo: Manole. 2002:447-71.
11. Ganança MM, Caovilla HH, Ganança FF, Munhoz MSL, Silva MLG. Vertigem posicional paroxística benigna. In: Silva MLG, Munhoz MSL, Ganança MM, Caovilla HH. Quadros clínicos otoneurológicos mais comuns. São Paulo: Atheneu; 2000. p 9-19.
12. do Rego André AP, Moriguti JC, Moreno NS. Conduct after Epley's maneuver in elderly with posterior canal BPPV in the posterior canal. Brazilian journal of otorhinolaryngology. 2010 May 1;76(3):300-5. Link
13. S. Ritchie, J. Corcoran, M. Liston, G. Jones. The Prevalence of Benign Paroxysmal Positional Vertigo (BPPV) in an Outpatient Physiotherapy Setting for Older Adults. Physiotherapy 2015; Volume 101, Supplement 1 eS1238–eS1642
16. Cohen HS, Jerabek J. Efficacy of treatments for posterior canal benign paroxysmal positional vertigo. The Laryngoscope. 1999 Apr;109(4):584-90. Link
17. Kanashiro AM, Pereira CB, Melo AC, Scaff M. Diagnóstico e tratamento das principais síndromes vestibulares. Arq Neuropsiquiatr. 2005;63(1):140-4. Link
18. Li S, Tian L, Han Z, Wang J. Impact of postmaneuver sleep position on recurrence of benign paroxysmal positional vertigo. PloS one. 2013 Dec 18;8(12):e83566. Link
19. Shim DB, Kim JH, Park KC, Song MH, Park HJ. Correlation between the head lying side during sleep and the affected side by benign paroxysmal positional vertigo involving the posterior or horizontal semicircular canal. The Laryngoscope. 2012 Apr;122(4):873-6. Link
20. Lopez-Escámez JA, Gámiz MJ, Fiñana MG, Perez AF, Canet IS. Position in bed is associated with left or right location in benign paroxysmal positional vertigo of the posterior semicircular canal. American journal of otolaryngology. 2002 Sep 1;23(5):263-6. Link
21. Çakir BÖ, Ercan I, Cakir ZA, Civelek, Turgut S. Relationship between the affected ear in benign paroxysmal positional vertigo and habitual head-lying side during bedrest. The Journal of Laryngology & Otology. 2006 Jul;120(7):534-6. Link
22. Korres SG, Papadakis CE, Riga MG, Balatsouras DG, Dikeos DG, Soldatos CR. Sleep position and laterality of benign paroxysmal positional vertigo. The Journal of Laryngology & Otology. 2008 Dec;122(12):1295-8. Link
23. Sato G, Sekine K, Matsuda K, Takeda N. Effects of sleep position on time course in remission of positional vertigo in patients with benign paroxysmal positional vertigo. Acta oto-laryngologica. 2012 Jun 1;132(6):614-7. Link
24. Pereira CB, Scaff M. Vertigem de posicionamento paroxística benigna. Arq Neuropsiquiatr. 2001;59(2-B):466-70. Link
25. Webster G, Sens PM, Salmito MC, Cavalcante JD, Santos PR, Silva AL, Souza ÉC. Hyperinsulinemia and hyperglycemia: risk factors for recurrence of benign paroxysmal positional vertigo. Brazilian journal of otorhinolaryngology. 2015 Aug;81(4):347-51. Link
26. Schuknecht HF. Cupulolithiasis. Arch Otolaryngol. 1969;90:765-78.
27. Schunecht HF, Ruby RR. Cupulolithiasis. Adv Otorhinolaryngol. 1973;20:434-43.
28. Korres SG, Balatsouras DG. Diagnostic, pathophysiologic, and therapeutic aspects of benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 2004 Oct;131(4):438-44. Link
29. Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 1992 Sep;107(3):399-404. Link
30. Katsarkas A. Benign paroxysmal positional vertigo (BPPV): idiopathic versus post-traumatic. Acta oto-laryngologica. 1999 Jan 1;119(7):745-9. Link
31. Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). Cmaj. 2003 Sep 30;169(7):681-93. Link
32. Hughes CA, Proctor L. Benign paroxysmal positional vertigo. The Laryngoscope. 1997 May;107(5):607-13. Link
33. Ganança MM, Caovilla HH, Munhoz MS, Silva ML, Ganança FF, Ganança CF. Como diagnosticar e tratar as vestibulopatias mais frequentes. Rev Bras Méd Cad Otorrinol. 2000 Dec;57(12).
34. Hain TC. Benign paroxysmal positional vertigo. Chicago, ILL: Northwestern University Medical School. Link
35. Zhang D, Zhang S, Zhang H, Xu Y, Fu S, Yu M, Ji P. Evaluation of vertebrobasilar artery changes in patients with benign paroxysmal positional vertigo. Neuroreport. 2013 Sep 11;24(13):741-5. Link
36. Fife TD, von Brevern M. Benign paroxysmal positional vertigo in the acute care setting. Neurologic clinics. 2015 Aug 1;33(3):601-17. Link
37. Haynes DS, Resser JR, Labadie RF, Girasole CR, Kovach BT, Scheker LE, Walker DC. Treatment of benign positional vertigo using the semont maneuver: efficacy in patients presenting without nystagmus. The Laryngoscope. 2002 May;112(5):796-801. Link
38. Koh G, Kunasaigaran G, Tan D. Benign positional paroxysmal vertigo (BPPV): impact of symptoms and physiotherapy management. Physiotherapy. 2015 May 1;101:e775-6. Link
39. Lopez-Escamez JA, Molina MI, Gamiz MJ, Fernandez-Perez AJ, Gomez M, Palma MJ, Zapata C. Multiple positional nystagmus suggests multiple canal involvement in benign paroxysmal positional vertigo. Acta oto-laryngologica. 2005 Jan 1;125(9):954-61. Link
40. Korres SG, Balatsouras DG. Diagnostic, pathophysiologic, and therapeutic aspects of benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 2004 Oct;131(4):438-44. Link
41. Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). Cmaj. 2003 Sep 30;169(7):681-93. Link
42. Bhattacharyya N, Gubbels SP, Schwartz SR, et al. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo (Update). Otolaryngol Head Neck Surg. 2017 Mar. 156 (3_suppl):S1-S47.
43. Garcia J. New guidelines for benign paroxysmal positional vertigo. Medscape Medical News. 2017 Mar 1.
44. Bhattacharyya N, Baugh RF, Orvidas L, et al. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 2008 Nov. 139(5 Suppl 4):S47-81.
45. S. Ritchie, J. Corcoran, M. Liston, G. Jones. The Prevalence of Benign Paroxysmal Positional Vertigo (BPPV) in an Outpatient Physiotherapy Setting for Older Adults. Physiotherapy 2015; Volume 101, Supplement 1 eS1238–eS1642
46. Gordon CR, Zur O, Furas R, Kott E, Gadoth N. Pitfalls in the diagnosis of benign paroxysmal positional vertigo. Harefuah. 2000 Jun;138(12):1024-7. Link
47. Labuguen RH. Initial evaluation of vertigo. Am Fam Physician. 2006 Jan 15;73(2):244-51. Link
49. Dix M, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Link
50. Herdman SJ, Tusa RJ. Avaliação e tratamento dos pacientes com vertigem posicional paroxística benigna. Reabilitação Vestibular, 2ª ed., São Paulo: Manole. 2002:447-71.
51. dos Santos Silva AL, Marinho MR, de Vasconcelos Gouveia FM, Silva JG, de Sá Ferreira A, Cal R. Benign Paroxysmal Positional Vertigo: comparison of two recent international guidelines. Brazilian journal of otorhinolaryngology. 2011 Mar 1;77(2):191-200. Link
52. Li J, Guo P, Tian S, Li K, Zhang H. Quick repositioning maneuver for horizontal semicircular canal benign paroxysmal positional vertigo. Journal of otology. 2015 Sep 1;10(3):115-7. Link
53. von Brevern M. Benign paroxysmal positional vertigo. Semin Neurol. 2013;33:204–211
54. Anagnostou E, Kouzi I, Spengos K. Diagnosis and treatment of anterior-canal benign paroxysmal positional vertigo: a systematic review. Journal of Clinical Neurology. 2015 Jul 1;11(3):262-7. Link
55. John C Li. Benign Paroxysmal Positional Vertigo Workup. Link
56. Sakata E, Ohtsu K, Itoh Y. Positional nystagmus of benign paroxysmal type (BPPN) due to cerebellar vermis lesions: pseudo-BPPN. Acta Oto-Laryngologica. 1991 Jan 1;111(sup481):254-7. Link
57. Dunniway HM, Welling DB. Intracranial tumors mimicking benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 1998 Apr;118(4):429-36. Link
58. Brandt T, Bronstein AM. Cervical vertigo J Neurol Neurosurg Psychiatry 2001;71:8-12
60. Steenerson RL, Cronin GW, Marbach PM. Effectiveness of treatment techniques in 923 cases of benign paroxysmal positional vertigo. The Laryngoscope. 2005 Feb;115(2):226-31. Link
61. Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 1992 Sep;107(3):399-404. Link
62. Richard W, Bruintjes TD, Oostenbrink P, van Leeuwen RB. Efficacy of the Epley maneuver for posterior canal BPPV: a long-term, controlled study of 81 patients. Ear, nose & throat journal. 2005 Jan;84(1):22-5. Link
64. Macias JD, Ellensohn A, Massingale S, Gerkin R. Vibration with the canalith repositioning maneuver: a prospective randomized study to determine efficacy. The Laryngoscope. 2004 Jun;114(6):1011-4. Link
65. Hain TC, Helminski JO, Reis IL, Uddin MK. Vibration does not improve results of the canalith repositioning procedure. Archives of Otolaryngology–Head & Neck Surgery. 2000 May 1;126(5):617-22. Link
66. Vaz DP, Gazzola JM, Lança SM, Dorigueto RS, Kasse CA. Clinical and functional aspects of body balance in elderly subjects with benign paroxysmal positional vertigo. Brazilian journal of otorhinolaryngology. 2013 Apr;79(2):150-7. Link
67. Fife TD. Recognition and management of horizontal canal benign positional vertigo. The American journal of otology. 1998 May;19(3):345-51. Link
68. Casani AP, Vannucci G, Fattori B, Berrettini S. The treatment of horizontal canal positional vertigo: our experience in 66 cases. The Laryngoscope. 2002 Jan;112(1):172-8. Link
69. Baloh RW, Jacobson K, Honrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993 Dec 1;43(12):2542-. Link
70. Lempert T, Tiel?Wilck K. A positional maneuver for treatment of horizontal canal benign positional vertigo. The Laryngoscope. 1996 Apr;106(4):476-8. Link
71. Massoud EA, Ireland DJ. Post-treatment instructions in the nonsurgical management of benign paroxysmal positional vertigo. The Journal of otolaryngology. 1996 Apr;25(2):121-5. Link
72. Roberts RA, Gans RE, DeBoodt JL, Lister JJ. Treatment of benign paroxysmal positional vertigo: necessity of postmaneuver patient restrictions. Journal of the American Academy of Audiology. 2005 Jun 1;16(6):357-66. Link
73. Rabie AN, Foster CA. Canalith-repositioning maneuvers. eMedicine Neurologic Procedures. 2010. Link
74. Humphriss RL, Baguley DM, Sparkes V, Peerman SE, Moffat DA. Contraindications to the Dix-Hallpike manoeuvre: A multidisciplinary review: Contraindicaciones de la maniobra de Dix-Hallpike: Una revisión multidisciplinaria. International journal of audiology. 2003 Jan 1;42(3):166-73. Link
75. Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Archives of Otolaryngology. 1980 Aug 1;106(8):484-5. Link
76. Brandt T, Huppert D, Hecht J, Karch C, Strupp M. Benign paroxysmal positioning vertigo: a long-term follow-up (6–17 years) of 125 patients. Acta oto-laryngologica. 2006 Jan 1;126(2):160-3. Link
77. Simhadri S, Panda N, Raghunathan M. Efficacy of particle repositioning maneuver in BPPV: a prospective study. American journal of otolaryngology. 2003 Nov 1;24(6):355-60. Link
78. Do YK, Kim J, Park CY, Chung MH, Moon IS, Yang HS. The effect of early canalith repositioning on benign paroxysmal positional vertigo on recurrence. Clinical and experimental otorhinolaryngology. 2011 Sep;4(3):113. Link
79. Steenerson RL, Cronin GW, Marbach PM. Effectiveness of treatment techniques in 923 cases of benign paroxysmal positional vertigo. The Laryngoscope. 2005 Feb;115(2):226-31. Link
80. Epley JM. The canalith repositioning procedure: for treatment of benign paroxysmal positional vertigo. Otolaryngology—Head and Neck Surgery. 1992 Sep;107(3):399-404. Link
81. Brandt T, Huppert D, Hecht J, Karch C, Strupp M. Benign paroxysmal positioning vertigo: a long-term follow-up (6–17 years) of 125 patients. Acta oto-laryngologica. 2006 Jan 1;126(2):160-3. Link
82. Evidence-Based Medicine Consult. Procedure: Epley Maneuver (Canalith Repositioning Procedure, CRP).
Link
83. Evidence-Based Medicine Consult. Procedure: Lempert Roll. Link
84. Takasaki H, Johnston V, Treleaven J, Pereira M, Jull G. Driving with a chronic whiplash-associated disorder: a review of patients' perspectives. Archives of physical medicine and rehabilitation. 2011 Jan 1;92(1):106-10. Link
85. Ojala M, Palo J. The aetiology of dizziness and how to examine a dizzy patient. Annals of medicine. 1991 Jan 1;23(3):225-30. Link
86. Stenger HH. Análisis del vertigo; exploración del nystagmo espontáneo y del provocado. Tratado de otorrinolaringologia. Barcelona: Editorial Cientifico Médica. 1969:603-46.
87. Wrisley DM, Sparto PJ, Whitney SL, Furman JM. Cervicogenic dizziness: a review of diagnosis and treatment. Journal of Orthopaedic & Sports Physical Therapy. 2000 Dec;30(12):755-66. Link
88. Phillipszoon AJ. Neck torsion nystagmus. Pract Oto-Rhi- no-Laryngologist. 1963;25:339-344.
89. Huijbregts P, Vidal P. Dizziness in orthopaedic physical therapy practice: Classification and pathophysiology. Journal of Manual & Manipulative Therapy. 2004 Oct 1;12(4):199-214. Link
90. Norre ME, Stevens A. Cervical vertigo. Acta Oto-Rhino-Larynologica Belgica 1987; 41(3):436-52
91. Fitz-Ritson D. Assessment of cervicogenic vertigo. J Manipulative Physiol Ther. 1991 Mar-Apr;14(3):193-8.
92. Côté P, Mior SA, Fitz-Ritson D. Cervicogenic vertigo: a report of three cases. The Journal of the Canadian Chiropractic Association. 1991 Jun;35(2):89. Link
93. Weiner HL, Levitt LP. Neurology for the House Officer. 4th ed. Baltimore: Williams and Wilkens, 1989.
94. Foster CA, Ponnapan A, Zaccaro K, Strong D. A comparison of two home exercises for benign positional vertigo: Half somersault versus Epley Maneuver. Audiology and Neurotology Extra. 2012;2(1):16-23. Link
95. Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol. 2007;20(1):40–46.
96. Neuhauser HK, Von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T. Epidemiology of vestibular vertigo: a neurotologic survey of the general population. Neurology. 2005 Sep 27;65(6):898-904. Link
97. Shim DB, Song CE, Jung EJ, Ko KM, Park JW, Song MH. Benign paroxysmal positional vertigo with simultaneous involvement of multiple semicircular canals. Korean journal of audiology. 2014 Dec;18(3):126. Link
98. Korpon JR, Sabo RT, Coelho DH. Barometric pressure and the incidence of benign paroxysmal positional vertigo. American journal of otolaryngology. 2019 May 15. Link
99. Chen J, Zhang S, Cui K, Liu C. Risk factors for benign paroxysmal positional vertigo recurrence: a systematic review and meta-analysis. Journal of Neurology. 2020 Aug 24:1-1. Link
100. Bruss D, Abouzari M, Sarna B, Goshtasbi K, Lee A, Birkenbeuel J, Djalilian HR. Migraine Features in Patients With Recurrent Benign Paroxysmal Positional Vertigo. Otology & Neurotology: Official Publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2020 Dec 10. Link
101. Guerra J, Devesa J. Melatonin Exerts Anti-Inflammatory, Antioxidant, and Neuromodulatory Effects That Could Potentially Be Useful in the Treatment of Vertigo. International Journal of Otolaryngology. 2021 Mar 23;2021. Link
102. Laurent G, Vereeck L, Verbecque E, Herssens N, Casters L, Spildooren J. Effect of age on treatment outcomes in benign paroxysmal positional vertigo: A systematic review. Journal of the American Geriatrics Society. 2021 Oct 26.
103. Ke Y, Ma X, Jing Y, Diao T, Yu L. Risk factors for residual dizziness in patients with benign paroxysmal positional vertigo after successful repositioning: a systematic review and meta-analysis. European Archives of Oto-Rhino-Laryngology. 2022 Feb 26:1-20. Link
104. Sharif S, Khoujah D, Greer A, Naples JG, Upadhye S, Edlow JA. Vestibular Suppressants for Benign Paroxysmal Positional Vertigo: A Systematic Review and Meta‐analysis of Randomized Controlled Trials. Academic Emergency Medicine. 2022 Oct 21. Link