Chiropractic Outcomes & Patient Satisfaction Synopsis
Dr. Tim Bertelsman - September 22, 2021
Purpose
The following synopsis details how the chiropractic profession ranks in terms of four key healthcare performance indicators.
Patient satisfaction
Clinical outcomes (Results)
Cost-effectiveness
Safety
Source
*Data for this 2021 COPS synopsis comes from the 2021 ChiroUp network dataset (1) – an analysis of 631,970 clinical diagnoses collected from more than 2,200 evidence-based chiropractic providers between July 2019 and June 2021, plus additional comparison data as referenced below. Patient satisfaction and clinical outcome metrics were derived from an emailed anonymous follow-up questionnaire sent to all patients (20.01% response rate).
Part 1: Patient Satisfaction
Overall Chiropractic Patient Satisfaction
Historically, the chiropractic profession has performed well in terms of patient satisfaction. (2-8) As far back as three decades ago, studies were documenting high levels of chiropractic patient satisfaction:
“Satisfaction levels with chiropractic care are quite high (83% of persons are satisfied or very satisfied). High satisfaction is related to several factors, including whether the chiropractor orders and interprets laboratory tests, whether the chiropractor displays concern about patient’s overall health and the extent to which the chiropractor explains the condition and the treatment.” (2)
More recent evidence from the 2021 ChiroUp network dataset suggests that chiropractic patient satisfaction levels remain high.
Patient Satisfaction Comparison by Provider Type
Patient satisfaction data suggests that chiropractors perform well relative to other healthcare providers. One study of 797 patients treated by either a chiropractor or family physician measured satisfaction in nine areas and found:
“With one exception, satisfaction was higher for patients attending chiropractors [as compared to family medicine physicians].” (8)
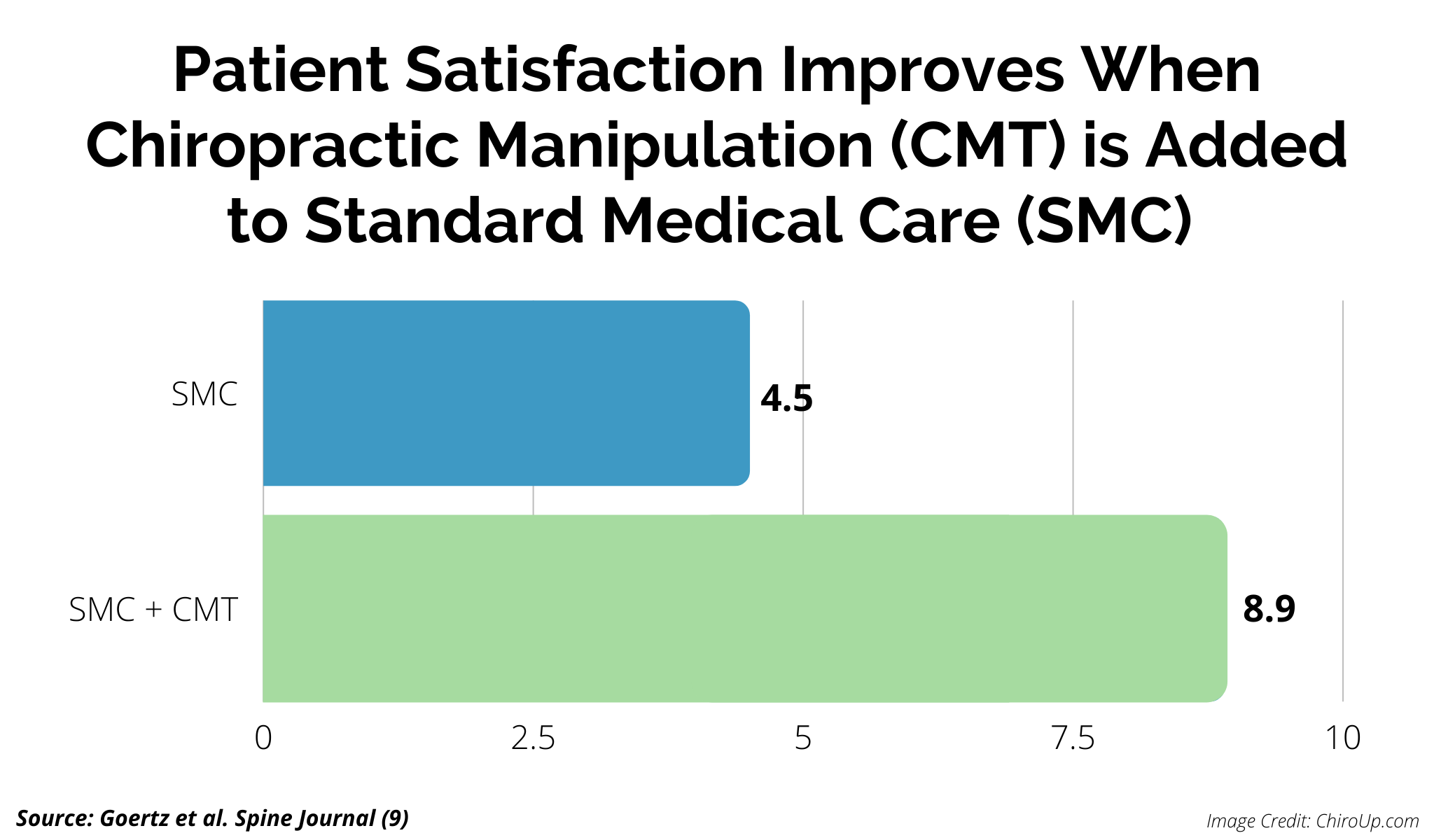
Another study found that patient satisfaction nearly doubled when chiropractic manipulation was added to standard medical care. (9)
Likelihood to Refer
A consumer’s likelihood to recommend a particular service or product is considered an essential prognosticator for the utility of any business. A standardized question for measuring this metric in healthcare is, “On a scale of 1-10, how likely are you to recommend this provider to others?”
The 2021 ChiroUp network dataset demonstrated that chiropractic patients are extremely likely to recommend their provider to others.
Overall Net Promoter Score (NPS)
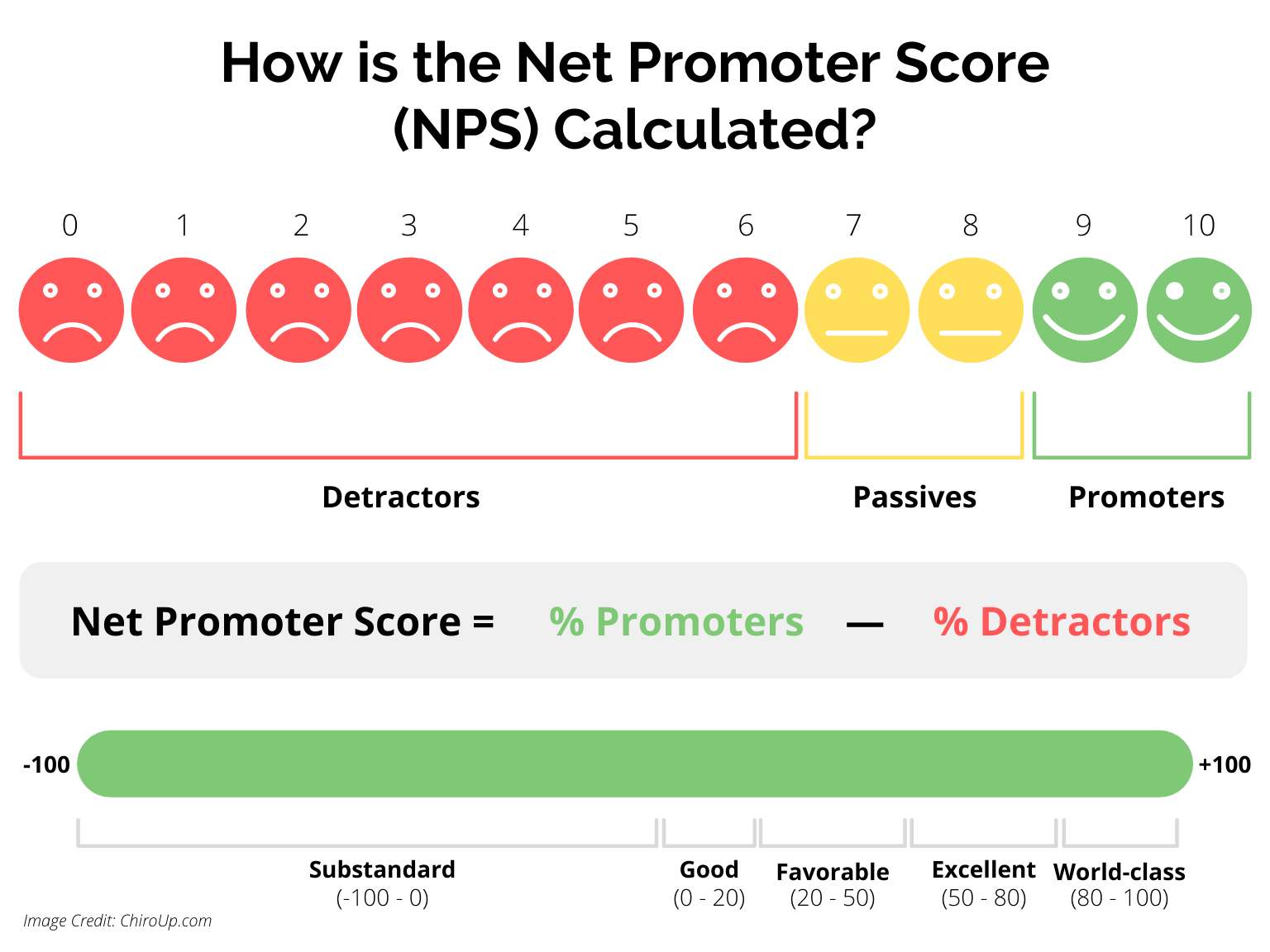
The Net Promoter Score (NPS) is the gold standard gauge of consumer satisfaction and loyalty. (10-12) A wide array of healthcare service providers have implemented the NPS survey to measure patient satisfaction. (13-18)
NPS scores for healthcare providers can be calculated from the likelihood that someone would recommend their provider to others (0-10 scale).
The 2021 ChiroUp network dataset found that, as a whole, chiropractors receive exceptionally high NPS scores from their patients.
Net Promoter Scores by Country
More than 90 countries have established chiropractic practices. (19,20) Direct access to chiropractic care is available in 90% of those countries, and the majority (51%) provide at least some degree of insurance reimbursement for chiropractic care. (20)
The following global breakdown illustrates that chiropractic patients worldwide share similar high levels of enthusiasm for recommending their chiropractors to others.
NPS Comparison by Provider Type
In general, NPS scores for the healthcare industry are favorable, averaging between 16 and 38. (21,22) NPS scores for primary care physicians average around 35. (23)
Chiropractors are primary care providers in many areas (24). However, their average NPS score differs from other PCP’s. The 2021 ChiroUp network dataset cumulative NPS score for chiropractors is 89.8, ranking among the highest in healthcare.
Online Satisfaction Reviews- Google
Online ratings provide another independent mechanism to gauge patient satisfaction. And an important one, since nearly three-quarters (71%) of patients now use online reviews as their first step in finding a new doctor. (25)
Consumer research has found that, in general, online reviews for healthcare providers (i.e., Google, Yelp, HealthGrades, etc.) tend to mirror the provider’s NPS score. (26,27) The 2021 ChiroUp network dataset supports that correlation.
An analysis of nearly 5000 providers found that the average medical physician’s online rating is 3.8 out of 5 possible stars. (28) An earlier and more comprehensive analysis by NPR placed that number slightly lower at 3.6. (29) In contrast, the 2021 ChiroUp network average Google rating for chiropractors is 4.9 out of 5.
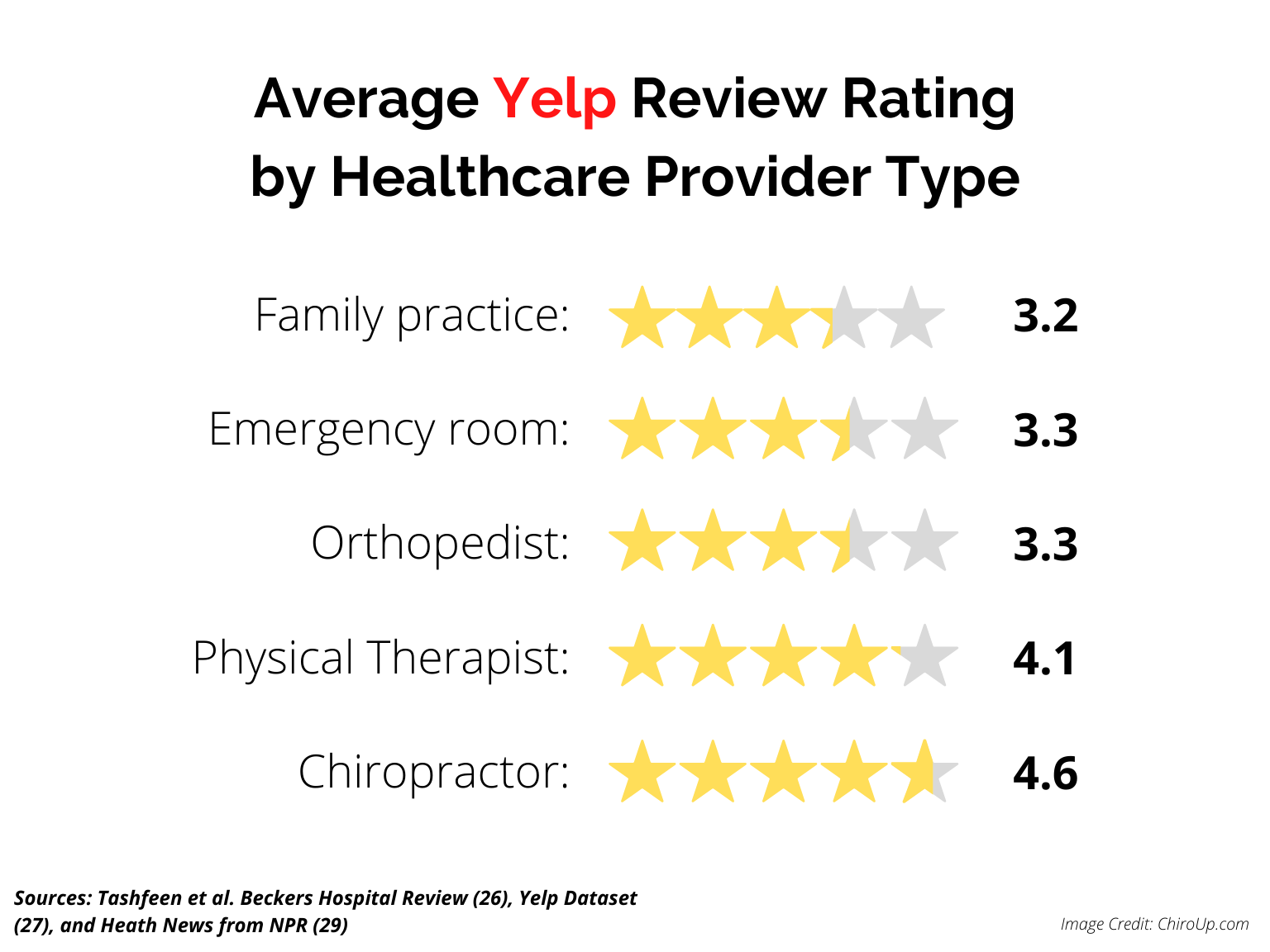
Online Satisfaction Reviews- Yelp
A more detailed analysis of the Yelp dataset reinforces the finding that, on average, online satisfaction ratings for chiropractic physicians are higher than other specialists. (25,27)
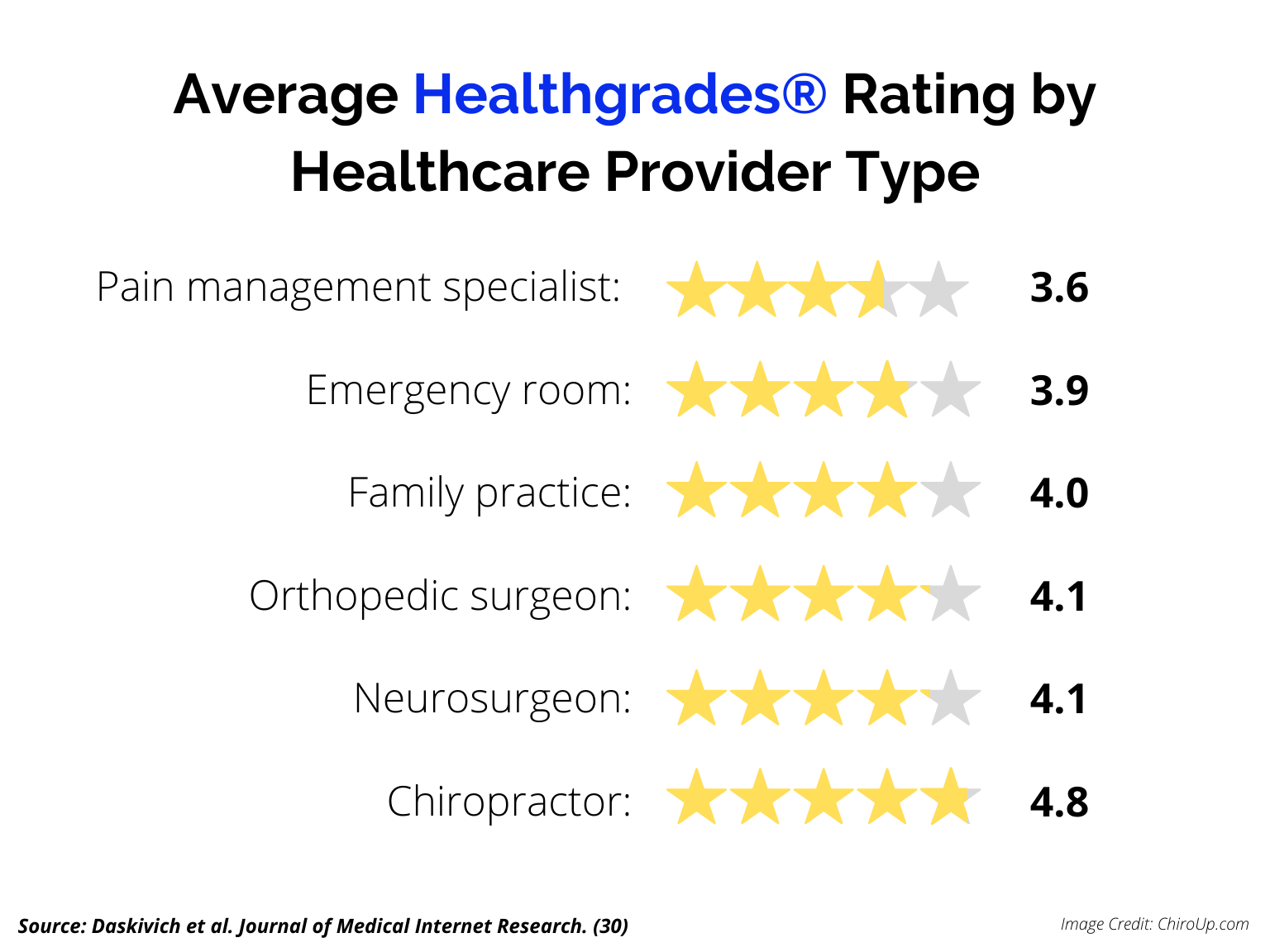
Online Satisfaction Reviews- Healthgrades
An analysis of Healthgrades® US consumer ratings for 212,933 health care providers found that chiropractors performed very well compared to medical specialists (4.0) and surgeons (4.2). (30)
Part 2: Chiropractic Diagnoses
Reasons to Visit a Chiropractor
The 2021 ChiroUp network dataset highlights the most common regional complaints in chiropractic offices.
* This 2021 COPS Synopsis data parallels findings from a 2017 scoping review (31) defining the frequency of common chiropractic presentations: Back conditions (49.7%), Neck conditions (22.5%), Extremity problems (10.0%), Non-musculoskeletal conditions (3.1%).
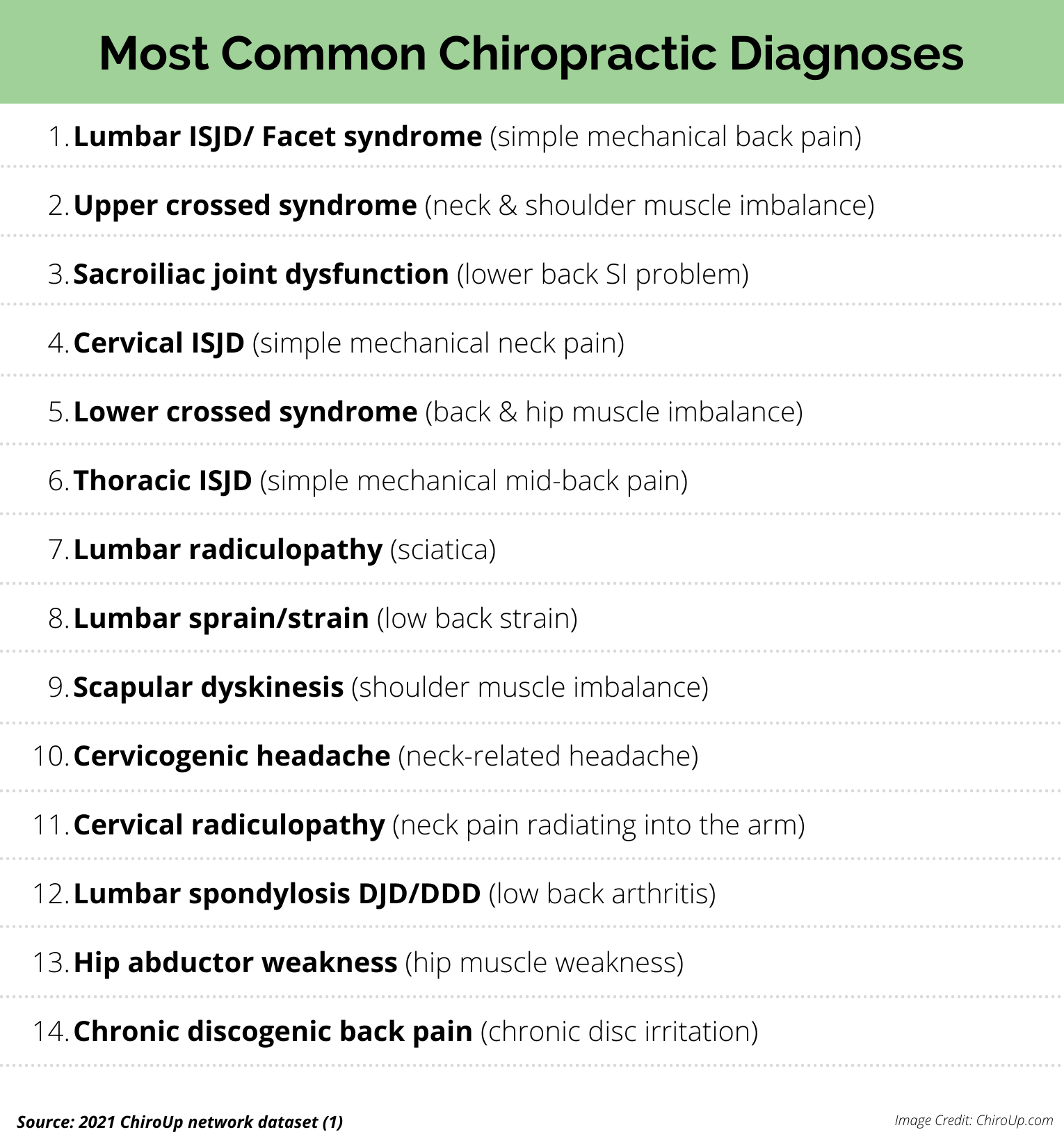
Top 10 Chiropractic Diagnoses
A more specific condition breakdown of the 2021 ChiroUp network dataset highlights the ten most common diagnoses made in chiropractic offices.
Most Common Spinal Diagnoses
Four out of five adults will experience neck or back pain that limits their daily activity at some point in their lifetime. (32,33) It should come as no surprise that spine-related diagnoses are the leading conditions in chiropractic offices. The 2021 ChiroUp network dataset provides a breakdown of the most common spinal diagnoses in chiropractic offices.
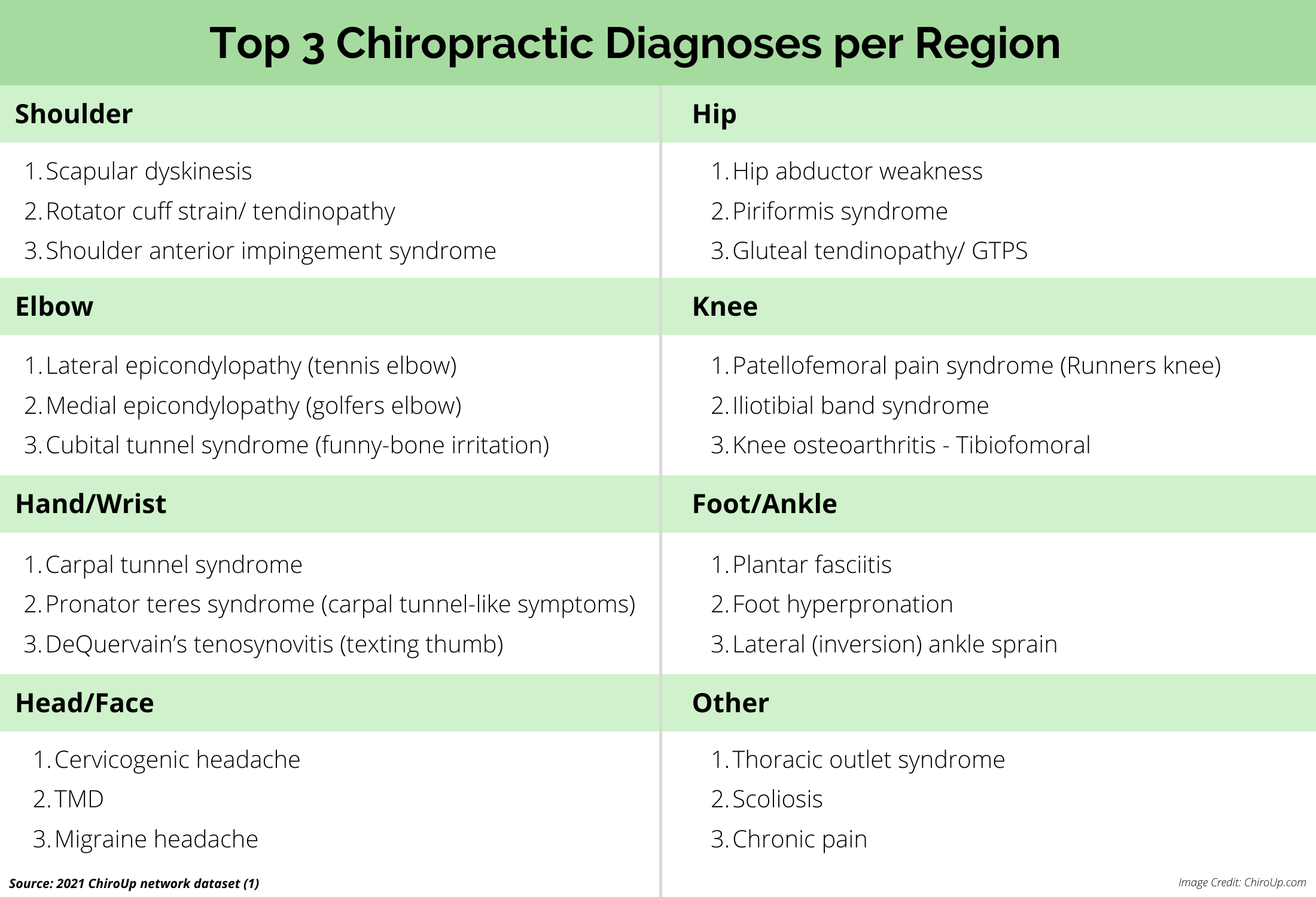
Top Diagnoses by Region
Chiropractors are trained to assess and treat various complaints outside of the spine, including problems ranging from headaches to plantar fasciitis. The following breakdown lists the three most common musculoskeletal diagnoses per region.
Treating Causes vs. Symptoms
Functional deficits (muscle imbalances) comprise four of the top fourteen diagnoses made in evidence-based chiropractic offices. Additionally, functional deficits represent more than 21% of all chiropractic diagnoses. This focus on identifying the underlying biomechanical cause (i.e. hip abductor weakness), as opposed to the more simplistic ICD-10-defined structural result (i.e. hip osteoarthritis), may help explain the above-average clinical outcomes shown in the subsequent section.
Part 3: Clinical Outcomes
Average Improvement
Results of the 2021 ChiroUp network dataset confirm that chiropractic patients experience significant average improvement within 30 days of initiating care.
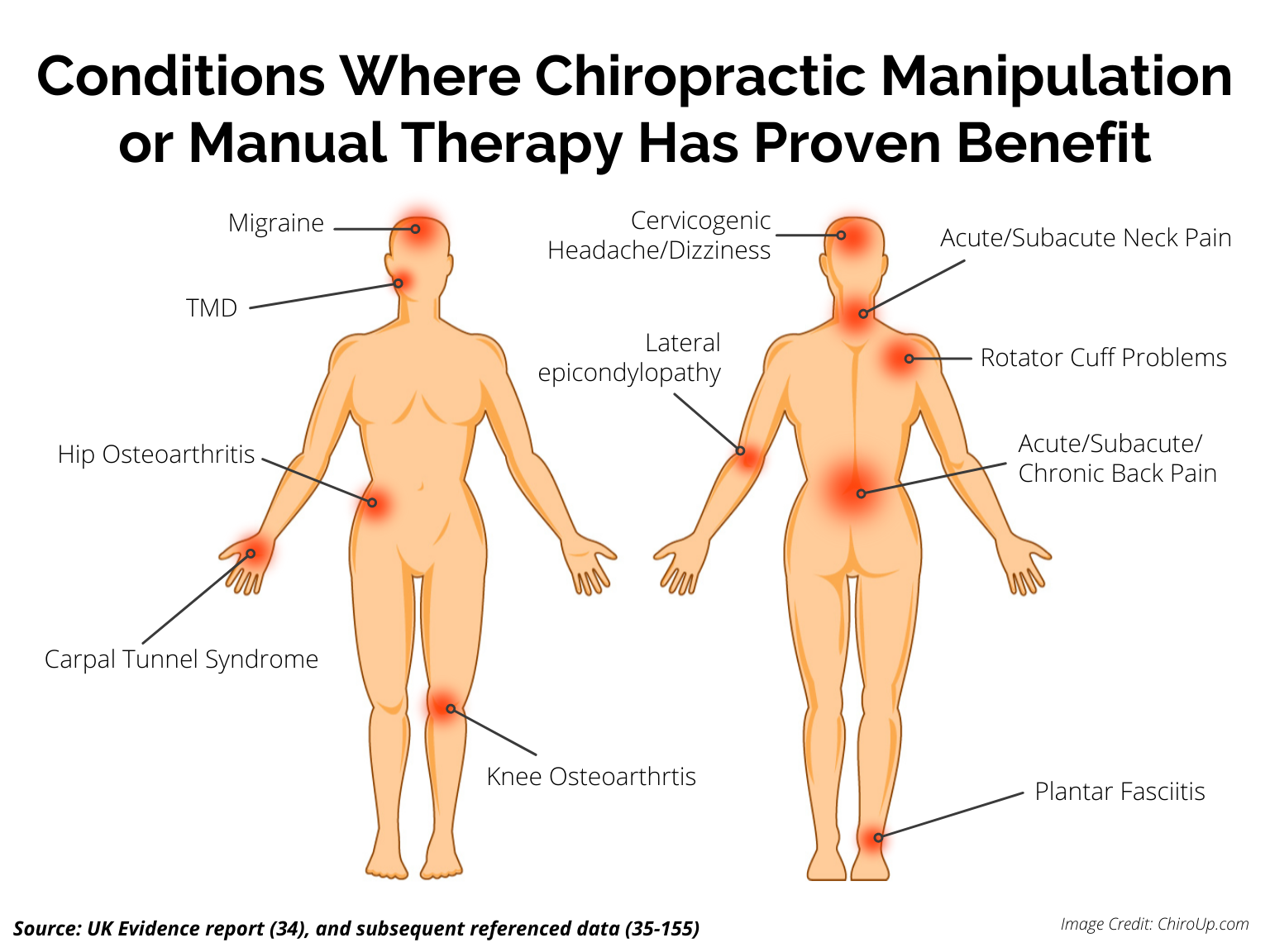
Chiropractic Effectiveness
Significant data has shown that chiropractic care, including spinal manipulation, is an effective solution for various musculoskeletal disorders.
The UK Evidence Report (34) provided a “comprehensive summary of the scientific evidence for manual therapy” and concluded that spinal manipulation/mobilization is effective in adults for the conditions listed below. Subsequent studies have confirmed these findings. (Additional references included)
Acute, subacute, and chronic low back pain (35-52)
Migraine (53-62)
Cervicogenic headache (63-76)
Cervicogenic dizziness (77-79)
Acute/subacute neck pain (41, 80-98)
Several extremity joint conditions (see below)
Other extensive studies have defined the specific extremity conditions where manipulation/mobilization has proven merit:
Rotator cuff problems (99-109)
Lateral epicondylopathy (tennis elbow) (100,110-122)
Carpal tunnel syndrome (123,124)
Hip and knee osteoarthritis (125-141)
Ankle sprains (99,142)
Plantar fasciitis (143-152)
TMD (jaw pain) (153-155)
Most Responsive Diagnoses
In recent years, the healthcare industry has focused on defining the most effective treatment for each condition. Evidence-based chiropractors concentrate on identifying the most amenable diagnoses and collaboratively referring conditions that lie outside of their expertise.
The 2021 ChiroUp network dataset defined conditions showing the greatest percent of average improvement after 30 days of initiating chiropractic care.
Outcomes By Provider Type
Multiple published studies have shown that chiropractors perform very well compared to other healthcare providers for musculoskeletal complaints. (8,9, 156-158) Studies comparing chiropractic or manual therapy clinical outcomes to standard medical care and physical therapy highlight a consistent theme:
The manual therapy group showed a faster improvement than the physiotherapy group and the general practitioner care group. (158)
[Low back manipulation] provides greater short-term reductions in self-reported disability and pain compared with usual medical care. (156)
One study compared 30-day low back pain outcomes of patients treated by chiropractors vs. those treated by MD/ family physicians and found:
Patients with chronic low-back pain treated by chiropractors showed greater improvement and satisfaction at one month than patients treated by family physicians. A higher proportion of chiropractic patients (56% vs. 13%) reported that their low-back pain was better or much better, whereas nearly one-third of medical patients reported their low-back pain was worse or much worse. (8)
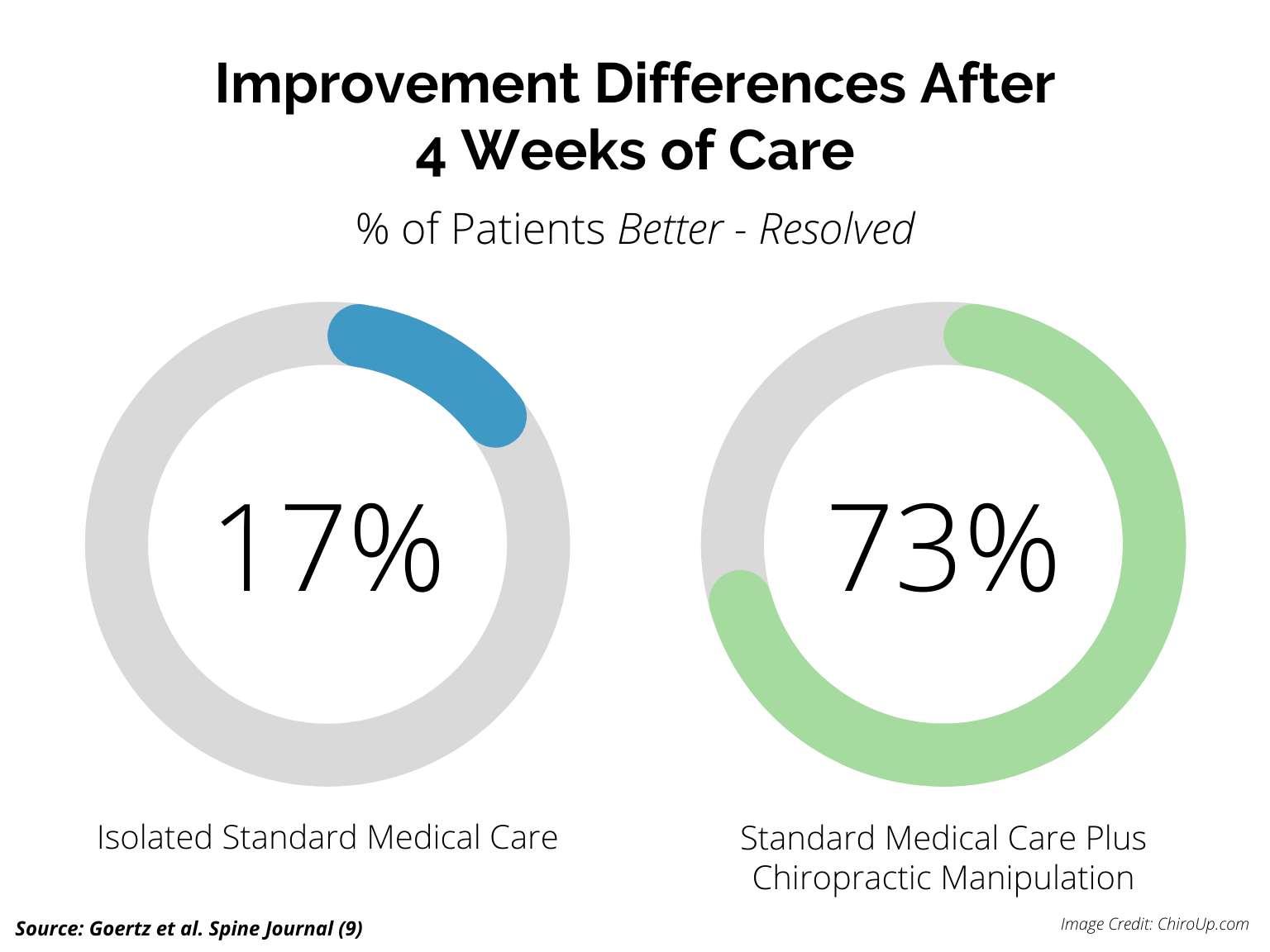
Collaborative Outcomes
Healthcare clinicians and researchers have found that adding chiropractic treatment to standard medical care for back pain resulted in less pain, less disability, improved function, lower use of pain medication, and higher satisfaction.
The results of this trial suggest that CMT [chiropractic manipulative therapy] in conjunction with SMC [standard medical care] offers a significant advantage for decreasing pain and improving physical functioning when compared with only standard care… 73% of participants in the SMC plus CMT group rated their global improvement as pain completely gone, much better, or moderately better, compared with 17% in the SMC group.”(9)
In response to abundant credible data regarding the utility of manipulation for back and neck pain, various medical authorities have endorsed spinal manipulation or conservative chiropractic care including, the American College of Physicians (159), US FDA (160), and US CDC. (161) One study highlights a growing theme:
“PCPs [primary care providers] utilizing an integrative medical approach emphasizing a variety of CAM therapies [complementary alternative medicine therapies, including chiropractic] had substantially improved clinical outcomes and cost offsets compared with PCPs utilizing conventional medicine alone.” (157)
Part 4: Cost-Effectiveness
Value
In the US alone, musculoskeletal pain, led by spinal disorders, is estimated to cost the healthcare system nearly one trillion dollars per year and is the most common cause of severe long-term pain and disability. (162)
Cost-effectiveness or value is a crucial metric for evaluating the merit of any treatment. The Value of any intervention for managing a specific condition is roughly calculated by dividing the clinical outcome by the cost of delivering that care.
Considering that evidence-based chiropractors deliver above-average clinical outcomes at low expense, consumers could expect their value to the healthcare system to be high. While the 2021 ChiroUp network dataset did not directly measure cost-effectiveness, multiple other studies have assessed that metric and concluded that chiropractic is highly cost effective (157, 158, 163,164,185-189) . The following sections summarize a small portion of that data.
Cost Comparison by Provider Type
An extensive systematic review (157) compared chiropractic care to standard medical care and physiotherapy for musculoskeletal pain and concluded:
Manual therapy techniques [including chiropractic manipulation] were more cost-effective than usual general practitioner care …for improving low back and shoulder pain/disability. (157)
Multiple other studies have come to the same conclusion:
A claims analysis of Blue Cross Blue Shield of Tennessee’s low back pain claims data showed that care initiated with a doctor of chiropractic (DC) saves nearly 40 percent on healthcare costs compared with care initiated through a medical doctor (MD). (163)
A cost analysis of various spine, hip, and shoulder problems treated by chiropractors vs. medical providers showed that mean treatment costs over four months were significantly lower in patients initially consulting a chiropractor. (164)
A British Medical Journal cost comparison for neck pain treatment costs found an even more significant disparity: “The total costs of manual therapy were around one-third of the costs of physiotherapy and general practitioner care.” (158)
Ancillary Costs – Healthcare Referrals
Healthcare expenditures rise when additional providers enter the clinical picture. The choice of initial provider plays a dramatic role in predicting the likelihood of future referrals, tests, and procedures.
Several studies have found that patients saw fewer total providers throughout their episode of care when treatment is initiated with a chiropractor. (165-167) Data from Optum Healthcare shows that spinal patients who initiate care with a chiropractor see an average of 1.7 different providers compared to 3.2 different providers for spinal patients starting with other specialties. (167)
Ancillary Costs – Surgery
The majority of musculoskeletal problems can be resolved without surgery. Many issues that were once thought to necessitate surgery are now being effectively managed conservatively. A 2020 study concluded that 97% of lumbar disc herniations are successfully managed nonoperatively. (168)
The choice of initial provider is significantly associated with the likelihood of subsequent surgery. A Spine journal study found that approximately 42.7% of injured workers who first saw a surgeon had surgery, in contrast to only 1.5% of those who saw a chiropractor. (166)
Ancillary Costs – Opioids & Other Drugs
Research shows that chemicals [drugs] are largely ineffective for managing mechanical musculoskeletal problems like back pain. (169-173) Even powerful medications including opioids, have questionable outcomes and undesired side effects. (173)
In addition to questionable benefits, opioids carry undeniable risks. In 2018, over 67,000 people died from drug overdoses – most (73%) from prescription opioid medicine. (174) And in the prior decade, overdose death rates and substance use rates increased 3-4 fold – in parallel to sales of prescription pain relievers. (175)
Recent studies have shown that chiropractic care is a natural solution that may help solve the opioid epidemic. A 2019 Pain Medicine journal systematic review found that patients participating in chiropractic care were 64% less likely to receive an opioid prescription than nonusers. (176)
A 2020 systematic review found that spinal pain patients who engaged with chiropractic care “had half the risk of filling an opioid prescription” over the next six years. (177)
Ancillary Costs – Hospitalization, Surgery & Medication
One 4-year study demonstrated that integrating complementary care, notably chiropractors, into standard medical care can substantially decrease healthcare expenditures (157):
Value to Healthcare Plans
Because of their ability to deliver high-value care with lower secondary costs, chiropractors become more appealing to patients and healthcare payors. An Optum analysis concluded that healthcare plans that formally incorporate chiropractic typically realize a 2:1 return for every dollar spent. (178)
Part 5: Safety
Spinal Manipulation Safety
Attitudes have changed as researchers have learned more about the safety of spinal manipulation. The Journal of the American Medical Association recently concluded “spinal manipulative therapy was associated with improvements in pain and function with only transient minor musculoskeletal harms.” (179)
Another landmark study found that “risk of injury to the head, neck or trunk within seven days was 76% lower among subjects with a chiropractic office visit as compared to those who saw a primary care physician.” (180)
Malpractice Claims Per Provider
Malpractice claims data reinforces the safety record of chiropractic care. An analysis of the National Practitioner Data Bank, Adverse Actions and Medical Malpractice Reports (1990-2017), and US Census Bureau defined the percentage of US malpractice claims by various provider types (181):
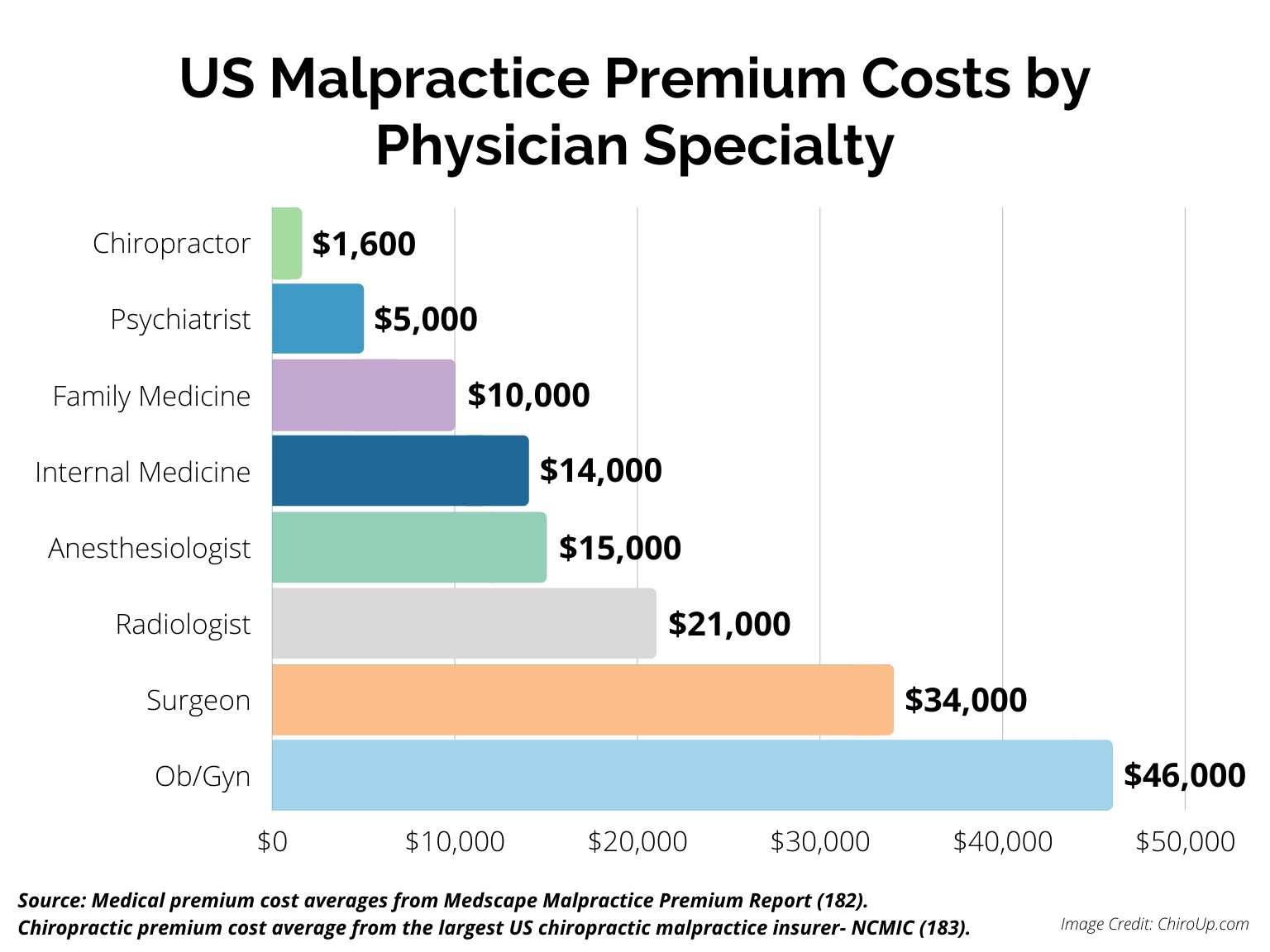
Malpractice Premium Costs Per Provider
The cost of insuring a provider is another reliable predictor of risk. An analysis of malpractice insurance premium rates per provider illustrates that chiropractors pay some of the lowest rates in healthcare (182,183):
Conclusion
This 2021 COPS synopsis confirms that chiropractors demonstrate above-average performance for the essential healthcare consumer needs. Evidence-based chiropractors should play a vital role in the future healthcare model because of their ability to safely and cost-effectively deliver excellent musculoskeletal clinical outcomes with high patient satisfaction.
Notes
The 2021 ChiroUp network dataset (1) summarized data from more than 2,200 evidence-based chiropractic practices (ChiroUp network). These providers share a common mission to achieve exceptional & timely clinical outcomes with high patient satisfaction by sharing and adhering to research-based best practices. Prior studies have shown that evidence-based chiropractors significantly outperform their non-evidence-based peers. (184) Hence, the outcomes reported in this study may not necessarily reflect the entire chiropractic profession.
About the Author
ChiroUp.com was founded in 2015 by Tim Bertelsman DC, CCSP, DACO and Brandon Steele DC, DACO. ChiroUp provides chiropractors with evidence-based resources to improve clinical outcomes and patient satisfaction. The platform is currently being used by over 2,000 chiropractors in fourteen different countries.
Reprints & Reproduction
To use this infographic or its data for any purpose, or to embed the graphic on another website, please include proper credit and link to the original article on chiroup.com
-
Bertelsman TJ, Steele BC, Gower JG. 2021 ChiroUp Network Dataset: Statistical Reporting of 631,970 Clinical Diagnoses Collected from 2212 Evidence-Based Chiropractic Providers Between July 2019- June 2021. Accessed on 07/30/2021 from Link
Sawyer CE, Kassak K. Patient satisfaction with chiropractic care. Journal of Manipulative and Physiological Therapeutics. 1993 Jan 1;16(1):25-32. Link
Gemmell HA, Hayes BM. Patient satisfaction with chiropractic physicians in an independent physicians’ association. Journal of manipulative and physiological therapeutics. 2001 Nov 1;24(9):556-9. Link
Hertzman-Miller RP, Morgenstern H, Hurwitz EL, Yu F, Adams AH, Harber P, Kominski GF. Comparing the satisfaction of low back pain patients randomized to receive medical or chiropractic care: results from the UCLA low-back pain study. American Journal of Public Health. 2002 Oct;92(10):1628-33. Link
Nyiendo J, Haas M, Goldberg B, Sexton G. Patient characteristics and physicians’ practice activities for patients with chronic low back pain: a practice-based study of primary care and chiropractic physicians. Journal of manipulative and physiological therapeutics. 2001 Feb 1;24(2):92-100. Link
Nyiendo J, Haas M, Goodwin P. Patient characteristics, practice activities, and one-month outcomes for chronic, recurrent low-back pain treated by chiropractors and family medicine physicians: a practice-based feasibility study. Journal of Manipulative and physiological Therapeutics. 2000 May 1;23(4):239-45. Link
Gaumer G. Factors associated with patient satisfaction with chiropractic care: survey and review of the literature. Journal of manipulative and physiological therapeutics. 2006 Jul 1;29(6):455-62. Link
Nyiendo J, Haas M, Goodwin P. Patient characteristics, practice activities, and one-month outcomes for chronic, recurrent low-back pain treated by chiropractors and family medicine physicians: a practice-based feasibility study. Journal of Manipulative and physiological Therapeutics. 2000 May 1;23(4):239-45. Link
Goertz CM, Long CR, Hondras MA, Petri R, Delgado R, Lawrence DJ, Owens EF, Meeker WC. Adding chiropractic manipulative therapy to standard medical care for patients with acute low back pain: results of a pragmatic randomized comparative effectiveness study. Spine. 2013 Apr 15;38(8):627-34. Link
QualtricsXM. What is NPS? Your ultimate guide to Net Promoter Score. QualtricsXM. Link
Reichheld FF. The one number you need to grow. Harvard business review. 2003 Dec 1;81(12):46-55.
Liyakasa K. Customer Experience Is Critical in Net Promoter Benchmarks. CRM Magazine. 2012 Jun;16(6):16-. Link
Stein N, Brooks K. A fully automated conversational artificial intelligence for weight loss: longitudinal observational study among overweight and obese adults. JMIR diabetes. 2017 Nov 1;2(2):e8590. Link
Wilberforce M, Batten E, Challis D, Davies L, Kelly MP, Roberts C. The patient experience in community mental health services for older people: a concept mapping approach to support the development of a new quality measure. BMC health services research. 2018 Dec;18(1):1-1. Link
Powell RE, Stone D, Hollander JE. Patient and health system experience with implementation of an enterprise-wide telehealth scheduled video visit program: mixed-methods study. JMIR medical informatics. 2018;6(1):e10. Link
Busby M, Matthews R, Burke F, Mullins A, Shumacher K. Is any particular aspect of perceived quality associated with patients tending to promote a dental practice to their friends and colleagues? Br Dent J. 2015;218(6):E12. doi:10.1038/sj.bdj.2015.229
Kinney WC. A simple and valuable approach for measuring customer satisfaction. Otolaryngology—Head and Neck Surgery. 2005 Aug;133(2):169-72. Link
Koladycz R, Fernandez G, Gray K, Marriott H. The Net Promoter Score (NPS) for insight into client experiences in sexual and reproductive health clinics. Global Health: Science and Practice. 2018 Oct 3;6(3):413-24. Link
NBCE. Practice Analysis of Chiropractic 2015. Chapter 1. National Board of Chiropractic Examiners. Link
Stochkendahl MJ, Rezai M, Torres P, Sutton D, Tuchin P, Brown R, Côté P. The chiropractic workforce: a global review. Chiropractic & manual therapies. 2019 Dec;27(1):1-9. Link
Grigore. What is a Good Net Promoter Score? (2021 NPS Benchmark). Retently. 2021 Apr. Link
VisitPay. What’s Your Score? Why Net Promoter Score Matters in Healthcare [ebook]. VisitPay. 2021 Mar. Link
WD Partners. Healthcare: Who Survives?. WD Partners Inc. 2019. Link
Shalen P. Primary Care Providers. Spine-Health. 2000 Nov. Link
Hedges L, Couey C. How Patients Use Online Reviews. Software Advice. 2020 Apr. Link
Tashfeen Ekram T. Healthcare NPS is high: How to make even more out of PX. Beckers Hospital Review. 2017 Dec. Link
Yelp dataset. Link
Kadry B, Chu LF, Kadry B, Gammas D, Macario A. Analysis of 4999 online physician ratings indicates that most patients give physicians a favorable rating. Journal of medical Internet research. 2011;13(4):e95. Link
Ornstein C. ProPublica. As reported in: Shots. Heath News from NPR. On Yelp, Doctors Get Reviewed Like Restaurants — And It Rankles. 08/06/2015. Accessed on 08/20/2021 at https://www.npr.org/sections/health-shots/2015/08/06/429624187/on-yelp-doctors-get-reviewed-like-restaurants-and-it-rankles
Daskivich T, Luu M, Noah B, Fuller G, Anger J, Spiegel B. Differences in online consumer ratings of health care providers across medical, surgical, and allied health specialties: observational study of 212,933 providers. Journal of medical Internet research. 2018 May 9;20(5):e9160. Link
Beliveau PJ, Wong JJ, Sutton DA, Simon NB, Bussières AE, Mior SA, French SD. The chiropractic profession: a scoping review of utilization rates, reasons for seeking care, patient profiles, and care provided. Chiropractic & manual therapies. 2017 Dec;25(1):1-7. Link
Sinnott PL, Dally SK, Trafton J, Goulet JL, Wagner TH. Trends in diagnosis of painful neck and back conditions, 2002 to 2011. Medicine. 2017 May;96(20). Link
Côté P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004 Dec 1;112(3):267-73. Link
Bronfort G, Haas M, Evans R, Leininger B, Triano J. Effectiveness of manual therapies: the UK evidence report. Chiropractic & osteopathy. 2010 Dec;18(1):1-33. Link
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2017 Apr 4;166(7):514-30. Link
Stochkendahl MJ, Kjaer P, Hartvigsen J, Kongsted A, Aaboe J, Andersen M, Andersen MØ, Fournier G, Højgaard B, Jensen MB, Jensen LD. National Clinical Guidelines for non-surgical treatment of patients with recent onset low back pain or lumbar radiculopathy. European Spine Journal. 2018 Jan 1;27(1):60-75. Link
Haldeman S, Dagenais S. What have we learned about the evidence-informed management of chronic low back pain?. The Spine Journal. 2008 Jan 1;8(1):266-77. Link
Chou R, Qaseem A, Snow V, Casey D, Cross JT, Shekelle P, Owens DK. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Annals of internal medicine. 2007 Oct 2;147(7):478-91. Link
von Heymann WJ, Schloemer P, Timm J, Muehlbauer B. Spinal high-velocity low amplitude manipulation in acute nonspecific low back pain: a double-blinded randomized controlled trial in comparison with diclofenac and placebo. Spine. 2013 Apr 1;38(7):540-8. Link
Cecchi F, Molino-Lova R, Chiti M, Pasquini G, Paperini A, Conti AA, Macchi C. Spinal manipulation compared with back school and with individually delivered physiotherapy for the treatment of chronic low back pain: a randomized trial with one-year follow-up. Clinical rehabilitation. 2010 Jan;24(1):26-36. Link
Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. The spine journal. 2004 May 1;4(3):335-56. Link
Dagenais S, Gay RE, Tricco AC, Freeman MD, Mayer JM. NASS contemporary concepts in spine care: spinal manipulation therapy for acute low back pain. The Spine Journal. 2010 Oct 1;10(10):918-40. Link
Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, Fu R, Brodt ED, Wasson N, Kantner S, Ferguson AJ. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Link
Giles LG, Muller R. Chronic spinal pain: a randomized clinical trial comparing medication, acupuncture, and spinal manipulation. Spine. 2003 Jul 15;28(14):1490-502. Link
Von Heymann WJ, Schloemer P, Timm J, Muehlbauer B. Spinal HVLA-manipulation in acute nonspecific LBP: A double blinded randomized controlled trial in comparison with diclofenac and placebo. Spine. 2012.
Bishop PB, Quon JA, Fisher CG, Dvorak MF. The Chiropractic Hospital-based Interventions Research Outcomes (CHIRO) study: a randomized controlled trial on the effectiveness of clinical practice guidelines in the medical and chiropractic management of patients with acute mechanical low back pain. The Spine Journal. 2010 Dec 1;10(12):1055-64. Link
Wilkey A, Gregory M, Byfield D, McCarthy PW. A comparison between chiropractic management and pain clinic management for chronic low-back pain in a national health service outpatient clinic. The Journal of Alternative and Complementary Medicine. 2008 Jun 1;14(5):465-73. Link
Parkin-Smith GF, Norman IJ, Briggs E, Angier E, Wood TG, Brantingham JW. A structured protocol of evidence-based conservative care compared with usual care for acute nonspecific low back pain: a randomized clinical trial. Archives of physical medicine and rehabilitation. 2012 Jan 1;93(1):11-20. Link
Aure OF, Nilsen JH, Vasseljen O. Manual therapy and exercise therapy in patients with chronic low back pain: a randomized, controlled trial with 1-year follow-up. Spine. 2003 Mar 15;28(6):525-31. Link
Paige NM, Miake-Lye IM, Booth MS, Beroes JM, Mardian AS, Dougherty P, Branson R, Tang B, Morton SC, Shekelle PG. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. Jama. 2017 Apr 11;317(14):1451-60. Link
Coulter ID, Crawford C, Hurwitz EL, Vernon H, Khorsan R, Booth MS, Herman PM. Manipulation and mobilization for treating chronic low back pain: a systematic review and meta-analysis. The Spine Journal. 2018 May 1;18(5):866-79. Link
Goertz CM, Long CR, Vining RD, Pohlman KA, Walter J, Coulter I. Effect of usual medical care plus chiropractic care vs usual medical care alone on pain and disability among US service members with low back pain: A comparative effectiveness clinical trial. JAMA network open. 2018 May 18;1(1):e180105-. Link
Astin JA, Ernst E. The effectiveness of spinal manipulation for the treatment of headache disorders: a systematic review of randomized clinical trials. Cephalalgia. 2002 Oct;22(8):617-23. Link
Rist PM, Bernstein C, Kowalski M, Osypiuk K, Connor JP, Vining R, Long CR, Macklin EA, Wayne PM. Multimodal chiropractic care for migraine: A pilot randomized controlled trial. Cephalalgia. 2020 Oct 13:0333102420963844. Link
Brønfort G, Nilsson N, Haas M, Evans RL, Goldsmith CH, Assendelft WJ, Bouter LM. Non-invasive physical treatments for chronic/recurrent headache. Cochrane Database of Systematic Reviews. 2004(3). Link
Rist PM, Hernandez A, Bernstein C, Kowalski M, Osypiuk K, Vining R, Long CR, Goertz C, Song R, Wayne PM. The Impact of Spinal Manipulation on Migraine Pain and Disability: A Systematic Review and Meta-Analysis. Headache: The Journal of Head and Face Pain. 2019 Apr;59(4):532-42. Link
Tuchin PJ, Pollard H, Bonello R. A randomized controlled trial of chiropractic spinal manipulative therapy for migraine. Journal of manipulative and physiological therapeutics. 2000 Feb 1;23(2):91-5. Link
Bryans R, Descarreaux M, Duranleau M, Marcoux H, Potter B, Ruegg R, Shaw L, Watkin R, White E. Evidence-based guidelines for the chiropractic treatment of adults with headache. Journal of manipulative and physiological therapeutics. 2011 Jun 1;34(5):274-89. Link
Harris SP. Chiropractic management of a patient with migraine headache. Journal of chiropractic medicine. 2005;4(1):25. Link
Biondi DM. Physical treatments for headache: a structured review. Headache: The Journal of Head and Face Pain. 2005 Jun;45(6):738-46. Link
Bronfort G, Assendelft WJ, Evans R, Haas M, Bouter L. Efficacy of spinal manipulation for chronic headache: a systematic review. Journal of manipulative and physiological therapeutics. 2001 Sep 1;24(7):457-66. Link
Noudeh YJ, Vatankhah N, Baradaran HR. Reduction of current migraine headache pain following neck massage and spinal manipulation. International journal of therapeutic massage & bodywork. 2012;5(1):5. Link
1 Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, Emberson J, Marschner I, Richardson C. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine. 2002 Sep 1;27(17):1835-43. Link
McCrory, Penzlen, Hasselblad, Gray. Duke Evidence Report (2001).
Antonia GC. Efficacy of manual and manipulative therapy in the perception of pain and cervical motion in patients with tension-type headache: a randomized, controlled clinical trial. Journal of chiropractic medicine. 2014 Mar 1;13(1):4-13. Link
Dunning JR, Butts R, Mourad F, Young I, Fernandez-de-las Peñas C, Hagins M, Stanislawski T, Donley J, Buck D, Hooks TR, Cleland JA. Upper cervical and upper thoracic manipulation versus mobilization and exercise in patients with cervicogenic headache: a multi-center randomized clinical trial. BMC musculoskeletal disorders. 2016 Dec;17(1):64. Link
Garcia JD, Arnold S, Tetley K, Voight K, Frank RA. Mobilization and manipulation of the cervical spine in patients with cervicogenic headache: any scientific evidence?. Frontiers in neurology. 2016 Mar 21;7:40. Link
Varatharajan S, Ferguson B, Chrobak K, Shergill Y, Cote P, Wong JJ, Yu H, Shearer HM, Southerst D, Sutton D, Randhawa K. Are non-invasive interventions effective for the management of headaches associated with neck pain? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. European spine journal. 2016 Jul 1;25(7):1971-99. Link
Malo-Urriés M, Tricás-Moreno JM, Estébanez-de-Miguel E, Hidalgo-García C, Carrasco-Uribarren A, Cabanillas-Barea S. Immediate Effects of Upper Cervical Translatoric Mobilization on Cervical Mobility and Pressure Pain Threshold in Patients With Cervicogenic Headache: A Randomized Controlled Trial. Journal of manipulative and physiological therapeutics. 2017 Nov 1;40(9):649-58. Link
Haas M, Bronfort G, Evans R, Schulz C, Vavrek D, Takaki L, Hanson L, Leininger B, Neradilek MB. Dose-response and efficacy of spinal manipulation for care of cervicogenic headache: a dual-center randomized controlled trial. The Spine Journal. 2018 Oct 1;18(10):1741-54. Link
Malo-Urriés M, Tricás-Moreno JM, Estébanez-de-Miguel E, Hidalgo-García C, Carrasco-Uribarren A, Cabanillas-Barea S. Immediate Effects of Upper Cervical Translatoric Mobilization on Cervical Mobility and Pressure Pain Threshold in Patients With Cervicogenic Headache: A Randomized Controlled Trial. Journal of manipulative and physiological therapeutics. 2017 Nov 1;40(9):649-58. Link
Skelly AC, Chou R, Dettori JR, Turner JA, Friedly JL, Rundell SD, Fu R, Brodt ED, Wasson N, Kantner S, Ferguson AJ. Noninvasive Nonpharmacological Treatment for Chronic Pain: A Systematic Review Update. Link
Fernandez M, Moore C, Tan J, Lian D, Nguyen J, Bacon A, Christie B, Shen I, Waldie T, Simonet D, Bussières A. Spinal manipulation for the management of cervicogenic headache: A systematic review and meta?analysis. European Journal of Pain. 2020 Jul 4. Link
Dunning J, Butts R, Zacharko N, Fandry K, Young I, Wheeler K, Day J, Fernández-de-las-Peñas C. Spinal manipulation and perineural electrical dry needling in patients with cervicogenic headache: a multi-center randomized clinical trial. The Spine Journal. 2020 Oct 13. Link
Abaspour O, Akbari M. Relationship between echogenicity of deep cervical muscles and pain laterality in subjects suffering from cervicogenic headache. CRANIO®. 2021 Jan 7:1-8. Link
Govind J, Bogduk N. Sources of Cervicogenic Headache Among the Upper Cervical Synovial Joints. Pain Med. 2021 Jan 23:pnaa469. doi: 10.1093/pm/pnaa469. Epub ahead of print. PMID: 33484154. Link
Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Manual therapy. 2005 Feb 1;10(1):4-13. Link
Yaseen K, Hendrick P, Ismail A, Felemban M, Alshehri MA. The effectiveness of manual therapy in treating cervicogenic dizziness: a systematic review. Journal of physical therapy science. 2018;30(1):96-102. Link
Jin X, Du HG, Qiao ZK, Huang Q, Chen WJ. The efficiency and safety of manual therapy for cervicogenic cephalic syndrome (CCS): A systematic review and meta-analysis. Medicine. 2021 Feb 26;100(8). Link
Vernon H, Humphreys K, Hagino C. Chronic mechanical neck pain in adults treated by manual therapy: a systematic review of change scores in randomized clinical trials. Journal of Manipulative and Physiological Therapeutics. 2007 Mar 1;30(3):215-27. Link
Korthals-de Bos IB, Müllner M, Hoving JL, van Tulder MW, Rutten-van Mölken MP, Adèr HJ, de Vet HC, Koes BW, Vondeling H, Bouter LM. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trialCommentary: Bootstrapping simplifies appreciation of statistical inferences. Bmj. 2003 Apr 26;326(7395):911-4. Link
Hoving JL, Koes BW, de Vet HC, van der Windt DA, Assendelft WJ, van Mameren H, Devillé WL, Pool JJ, Scholten RJ, Bouter LM. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain: a randomized, controlled trial. Annals of internal medicine. 2002 May 21;136(10):713-22. Link
Swenson RS. Therapeutic modalities in the management of nonspecific neck pain. Physical medicine and rehabilitation clinics of North America. 2003 Aug;14(3):605-27. Link
Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Annals of internal medicine. 2012 Jan 3;156(1_Part_1):1-0. Link
Leaver AM, Maher CG, Herbert RD, Latimer J, McAuley JH, Jull G, Refshauge KM. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Archives of physical medicine and rehabilitation. 2010 Sep 1;91(9):1313-8. Link
Puentedura EJ, Landers MR, Cleland JA, Mintken P, Huijbregts P, Fernandez-De-Las-Peñas C. Thoracic spine thrust manipulation versus cervical spine thrust manipulation in patients with acute neck pain: a randomized clinical trial. journal of orthopaedic & sports physical therapy. 2011 Apr;41(4):208-20. Link
Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, Sigurdsson G. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. journal of orthopaedic & sports physical therapy. 2012 Jan;42(1):5-18. Link
Walker MJ, Boyles RE, Young BA, Strunce JB, Garber MB, Whitman JM, Deyle G, Wainner RS. The effectiveness of manual physical therapy and exercise for mechanical neck pain: a randomized clinical trial. Spine. 2008 Oct 15;33(22):2371-8. Link
Boyles RE, Walker MJ, Young BA, Strunce JB, Wainner RS. The addition of cervical thrust manipulations to a manual physical therapy approach in patients treated for mechanical neck pain: a secondary analysis. journal of orthopaedic & sports physical therapy. 2010 Mar;40(3):133-40. Link
Martínez-Segura R, Fernández-de-las-Peñas C, Ruiz-Sáez M, López-Jiménez C, Rodríguez-Blanco C. Immediate effects on neck pain and active range of motion after a single cervical high-velocity low-amplitude manipulation in subjects presenting with mechanical neck pain: a randomized controlled trial. Journal of manipulative and physiological therapeutics. 2006 Sep 1;29(7):511-7. Link
Bernal-Utrera C, Gonzalez-Gerez JJ, Anarte-Lazo E, Rodriguez-Blanco C. Manual therapy versus therapeutic exercise in non-specific chronic neck pain: a randomized controlled trial. Trials. 2020 Dec;21(1):1-0. Link
Saayman L, Hay C, Abrahamse H. Chiropractic manipulative therapy and low-level laser therapy in the management of cervical facet dysfunction: a randomized controlled study. Journal of manipulative and physiological therapeutics. 2011 Mar 1;34(3):153-63. Link
Wong JJ, Shearer HM, Mior S, Jacobs C, Côté P, Randhawa K, Yu H, Southerst D, Varatharajan S, Sutton D, van der Velde G. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the OPTIMa collaboration. The Spine Journal. 2016 Dec 1;16(12):1598-630. Link
Gorrell LM, Beath K, Engel RM. Manual and instrument applied cervical manipulation for mechanical neck pain: a randomized controlled trial. Journal of manipulative and physiological therapeutics. 2016 Jun 1;39(5):319-29. Link
Wong JJ, Shearer HM, Mior S, Jacobs C, Côté P, Randhawa K, Yu H, Southerst D, Varatharajan S, Sutton D, van der Velde G. Are manual therapies, passive physical modalities, or acupuncture effective for the management of patients with whiplash-associated disorders or neck pain and associated disorders? An update of the Bone and Joint Decade Task Force on Neck Pain and Its Associated Disorders by the OPTIMa collaboration. The Spine Journal. 2016 Dec 1;16(12):1598-630. Link
Groeneweg R, van Assen L, Kropman H, Leopold H, Mulder J, Smits-Engelsman BC, Ostelo RW, Oostendorp RA, van Tulder MW. Manual therapy compared with physical therapy in patients with non-specific neck pain: a randomized controlled trial. Chiropractic & manual therapies. 2017 Dec;25(1):12. Link
Whalen W, Farabaugh RJ, Hawk C, Minkalis AL, Lauretti W, Crivelli LS, Wyatt L, Sheppard M, Walters SA. Best-Practice Recommendations for Chiropractic Management of Patients With Neck Pain. Journal of Manipulative and Physiological Therapeutics. 2019 Dec 20. Link
Bussieres AE, Stewart G, Al-Zoubi F, Decina P, Descarreaux M, Hayden J, Hendrickson B, Hincapie C, Page I, Passmore S, Srbely J. The treatment of neck pain–associated disorders and whiplash-associated disorders: a clinical practice guideline. Journal of manipulative and physiological therapeutics. 2016 Oct 1;39(8):523-64. Link
Southerst D, Yu H, Randhawa K, Côté P, D’Angelo K, Shearer HM, Wong JJ, Sutton D, Varatharajan S, Goldgrub R, Dion S. The effectiveness of manual therapy for the management of musculoskeletal disorders of the upper and lower extremities: a systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Chiropractic & manual therapies. 2015 Dec;23(1):1-7. Link
Crosbie J, Kilbreath SL, Hollmann L, York S. Scapulohumeral rhythm and associated spinal motion. Clinical biomechanics. 2008 Feb 1;23(2):184-92. Link
Strunce JB, Walker MJ, Boyles RE, Young BA. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. Journal of Manual & Manipulative Therapy. 2009 Dec 1;17(4):230-6. Link
Walser RF, Meserve BB, Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. Journal of Manual & Manipulative Therapy. 2009 Dec 1;17(4):237-46. Link
Muth S, Barbe MF, Lauer R, McClure P. The effects of thoracic spine manipulation in subjects with signs of rotator cuff tendinopathy. Journal of orthopaedic & sports physical therapy. 2012 Dec;42(12):1005-16. Link
Kardouni JR, Shaffer SW, Pidcoe PE, Finucane SD, Cheatham SA, Michener LA. Immediate changes in pressure pain sensitivity after thoracic spinal manipulative therapy in patients with subacromial impingement syndrome: a randomized controlled study. Manual therapy. 2015 Aug 1;20(4):540-6. Link
Haik MN, Alburquerque-Sendín F, Silva CZ, Siqueira-Junior AL, Ribeiro IL, Camargo PR. Scapular kinematics pre–and post–thoracic thrust manipulation in individuals with and without shoulder impingement symptoms: a randomized controlled study. journal of orthopaedic & sports physical therapy. 2014 Jul;44(7):475-87. Link
Boyles RE, Ritland BM, Miracle BM, Barclay DM, Faul MS, Moore JH, Koppenhaver SL, Wainner RS. The short-term effects of thoracic spine thrust manipulation on patients with shoulder impingement syndrome. Manual therapy. 2009 Aug 1;14(4):375-80. Link
Vinuesa-Montoya S, Aguilar-Ferrándiz ME, Matarán-Peñarrocha GA, Fernández-Sánchez M, Fernández-Espinar EM, Castro-Sánchez AM. A preliminary randomized clinical trial on the effect of cervicothoracic manipulation plus supervised exercises vs a home exercise program for the treatment of shoulder impingement. Journal of chiropractic medicine. 2017 Jun 1;16(2):85-93. Link
Belón-Perez P, Cuesta-Vargas AI. Immediate Effects of Thoracic Spine Manipulation Upon Shoulder Functionality in Patients With Sutured Rotator Cuff Repair: A Prospective Study. Journal of manipulative and physiological therapeutics. 2018 Sep 1;41(7):589-95. Link
Dunning J, Butts R, Fernández-de-Las-Peñas C, Walsh S, Goult C, Gillett B, Arias-Buria JL, Garcia J, Young IA. Spinal Manipulation and Electrical Dry Needling in Patients With Subacromial Pain Syndrome: A Multicenter Randomized Clinical Trial. Journal of Orthopaedic & Sports Physical Therapy. 2020 Aug 28(0):1-46. Link
Souza TA. Differential diagnosis and management for the chiropractor: protocols and algorithms. Jones & Bartlett Publishers; 2009 Oct 7.
Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. British journal of sports medicine. 2005 Jul 1;39(7):411-22. Link
Vicenzino B, Paungmali A, Buratowski S, Wright A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Manual therapy. 2001 Nov 1;6(4):205-12. Link
Cleland JA, Flynn TW, Palmer JA. Incorporation of manual therapy directed at the cervicothoracic spine in patients with lateral epicondylalgia: a pilot clinical trial. Journal of manual & manipulative therapy. 2005 Jul 1;13(3):143-51. Link
Cleland JA, Whitman JM, Fritz JM. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epicondylalgia: a retrospective analysis. Journal of Orthopaedic & Sports Physical Therapy. 2004 Nov;34(11):713-24. Link
Fernández-Carnero J, Fernández-de-las-Peñas C, Cleland JA. Immediate hypoalgesic and motor effects after a single cervical spine manipulation in subjects with lateral epicondylalgia. Journal of manipulative and physiological therapeutics. 2008 Nov 1;31(9):675-81. Link
Javier González-Iglesias, Joshua A. Cleland, Maria del Rosario Gutierrez-Vega, and Cesar Fernández-de-las-Peñas, Multimodal Management Of Lateral Epicondylalgia In Rock Climbers :A prospective Case Series J Manipulative Physiol Ther 2011;34:635-642. Manchanda G, Grover D. Effectiveness of movement with mobilization compared with manipulation of wrist in case of lateral epicondylitis. Indian Journal of Physiotherapy and Occupational Therapy-An International Journal. 2008;2(1):16-25. Link
Struijs PA, Damen PJ, Bakker EW, Blankevoort L, Assendelft WJ, van Dijk CN. Manipulation of the wrist for management of lateral epicondylitis: a randomized pilot study. Physical therapy. 2003 Jul 1;83(7):608-16. Link
Lucado AM, Dale RB, Vincent J, Day JM. Do joint mobilizations assist in the recovery of lateral elbow tendinopathy? A systematic review and meta-analysis. Journal of Hand Therapy. 2018 Apr 26. Link
Zunke P, Auffarth A, Hitzl W, Moursy M. The effect of manLinkual therapy to the thoracic spine on pain-free grip and sympathetic activity in patients with lateral epicondylalgia humeri. A randomized, sample sized planned, placebo-controlled, patient-blinded monocentric trial. BMC Musculoskeletal Disorders. 2020 Dec;21(1):1-1. Link
Reyhan AC, Sindel D, Dereli EE. The effects of Mulligan’s mobilization with movement technique in patients with lateral epicondylitis. Journal of Back and Musculoskeletal Rehabilitation. 2020 Jan 1(Preprint):1-9. Link
Zunke P, Auffarth A, Hitzl W, Moursy M. The effect of manual therapy to the thoracic spine on pain-free grip and sympathetic activity in patients with lateral epicondylalgia humeri. A randomized, sample sized planned, placebo-controlled, patient-blinded monocentric trial. BMC Musculoskeletal Disorders. 2020 Dec;21(1):1-1. Link
Ahmed A, Ibrar M, Arsh A, Wali S, Hayat S, Abass S. Comparing the effectiveness of Mulligan mobilization versus Cyriax approach in the management of patients with subacute lateral epicondylitis. Journal of the Pakistan Medical Association. 2020 Oct 15:1-1.
Page MJ, O’Connor D, Pitt V, Massy, Westropp N. Exercise and mobilisation interventions for carpal tunnel syndrome. Cochrane Database of Systematic Reviews. 2012(6). Link
Sault JD, Jayaseelan DJ, Mischke JJ, Post AA. The Utilization of Joint Mobilization As Part of a Comprehensive Program to Manage Carpal Tunnel Syndrome: A Systematic Review. Journal of Manipulative and Physiological Therapeutics. 2020 Aug 26. Link
Brantingham JW, Williams AM, Parkin-Smith GF, Weston P, Wood T. A controlled, prospective pilot study of the possible effects of chiropractic manipulation in the treatment of osteo-arthritis of the hip. European Journal Of Chiropractic. 2003;51(3):149-66.
Hoskins W, McHardy A, Pollard H, Windsham R, Onley R. Chiropractic treatment of lower extremity conditions: a literature review. Journal of manipulative and physiological therapeutics. 2006 Oct 1;29(8):658-71. Link
Brantingham JW, Bonnefin D, Perle SM, Cassa TK, Globe G, Pribicevic M, Hicks M, Korporaal C. Manipulative therapy for lower extremity conditions: update of a literature review. Journal of manipulative and physiological therapeutics. 2012 Feb 1;35(2):127-66. Link
MacDonald CW, Whitman JM, Cleland JA, Smith M, Hoeksma HL. Clinical outcomes following manual physical therapy and exercise for hip osteoarthritis: a case series. Journal of Orthopaedic & Sports Physical Therapy. 2006 Aug;36(8):588-99. Link
Brantingham JW, Globe GA, Cassa TK, Globe D, Pollard H, Lee F, Bates C, Jensen M, Mayer S, Korporaal C, de Luca K. Research & Science. A Single-Group Pre-Test, Post-Test Design Using Full Kinetic Chain Manipulative Therapy with Rehabilitation in the Treatment of 27 Patients with Hip Osteoarthritis. Journal of the American Chiropractic Association. 2010 Aug 1;47(6). Link
Brantingham JW, Globe GA, Cassa TK, Globe D, Pollard H, Lee F, Bates C, Jensen M, Mayer S, Korporaal C, de Luca K. Research & Science. A Single-Group Pre-Test, Post-Test Design Using Full Kinetic Chain Manipulative Therapy with Rehabilitation in the Treatment of 27 Patients with Hip Osteoarthritis. Journal of the American Chiropractic Association. 2010 Aug 1;47(6). Link
De Luca K, Pollard H, Brantingham J, Globe G, Cassa T. Chiropractic management of the kinetic chain for the treatment of hip osteoarthritis: an Australian case series. Journal of manipulative and physiological therapeutics. 2010 Jul 1;33(6):474-9. Link
Brantingham JW, Parkin-Smith G, Cassa TK, Globe GA, Globe D, Pollard H, deLuca K, Jensen M, Mayer S, Korporaal C. Full kinetic chain manual and manipulative therapy plus exercise compared with targeted manual and manipulative therapy plus exercise for symptomatic osteoarthritis of the hip: a randomized controlled trial. Archives of physical medicine and rehabilitation. 2012 Feb 1;93(2):259-67. Link
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, de la Barra SL, Baxter GD, Theis JC, Campbell AJ, MOA Trial Team. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis and Cartilage. 2013 Apr 1;21(4):525-34. Link
Zhang W, Moskowitz R, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis and Cartilage. 2008;16:137-162.
Poulsen E, Hartvigsen J, Christensen HW, Roos EM, Vach W, Overgaard S. Patient education with or without manual therapy compared to a control group in patients with osteoarthritis of the hip. A proof-of-principle three-arm parallel group randomized clinical trial. Osteoarthritis and Cartilage. 2013 Oct 1;21(10):1494-503. Link
French HP, Cusack T, Brennan A, Caffrey A, Conroy R, Cuddy V, FitzGerald OM, Gilsenan C, Kane D, O’Connell PG, White B. Exercise and manual physiotherapy arthritis research trial (EMPART) for osteoarthritis of the hip: a multicenter randomized controlled trial. Archives of physical medicine and rehabilitation. 2013 Feb 1;94(2):302-14. Link
Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, McGowan J, Towheed T, Welch V, Wells G, Tugwell P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis care & research. 2012 Apr;64(4):465-74. Link
De Luca K, Pollard H, Brantingham J, Globe G, Cassa T. A randomized controlled trial of chiropractic management of the lower limb kinetic chain for the treatment of hip osteoarthritis: a study protocol. Journal of chiropractic medicine. 2011 Jun 1;10(2):86-92. Link
Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M. OARSI recommendations for the management of hip and knee osteoarthritis: part III: Changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis and cartilage. 2010 Apr 1;18(4):476-99. Link
Vaarbakken K, Elisabeth Ljunggren A. Superior effect of forceful compared with standard traction mobilizations in hip disability?. Advances in physiotherapy. 2007 Jan 1;9(3):117-28. Link
Dwyer L, Parkin-Smith GF, Brantingham JW, Korporaal C, Cassa TK, Globe G, Bonnefin D, Tong V. Manual and manipulative therapy in addition to rehabilitation for osteoarthritis of the knee: assessor-blind randomized pilot trial. Journal of manipulative and physiological therapeutics. 2015 Jan 1;38(1):1-21. Link
Dimou ES, Brantingham JW, Wood T. A randomized, controlled trial (with blinded observer) of chiropractic manipulation and Achilles stretching vs. orthotics for the treatment of plantar fasciitis. Journal of the American Chiropractic Association. 2004 Sep 1;41(9). Link
Bleakley CM, McDonough SM, MacAuley DC. Some conservative strategies are effective when added to controlled mobilisation with external support after acute ankle sprain: a systematic review. Australian Journal of Physiotherapy. 2008 Jan 1;54(1):7-20. Link
Green T, Refshauge K, Crosbie J, Adams R. A randomized controlled trial of a passive accessory joint mobilization on acute ankle inversion sprains. Physical therapy. 2001 Apr 1;81(4):984-94. Link
Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. Journal of Orthopaedic & Sports Physical Therapy. 2002 Apr;32(4):166-73. Link
van der Wees PJ, Lenssen AF, Hendriks EJ, Stomp DJ, Dekker J, de Bie RA. Effectiveness of exercise therapy and manual mobilisation in acute ankle sprain and functional instability: a systematic review. Australian Journal of Physiotherapy. 2006 Jan 1;52(1):27-37. Link
Eisenhart AW, Gaeta TJ, Yens DP. Osteopathic manipulative treatment in the emergency department for patients with acute ankle injuries. The Journal of the American Osteopathic Association. 2003 Sep 1;103(9):417-21.
Loudon JK, Reiman MP, Sylvain J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med. 2014 Mar 1;48(5):365-70. Link
Fraser JJ, Saliba SA, Hart JM, Park JS, Hertel J. Effects of midfoot joint mobilization on ankle-foot morphology and function following acute ankle sprain. A crossover clinical trial. Musculoskeletal Science and Practice. 2020 Apr 1;46:102130. Link
Weerasekara I, Osmotherly P, Snodgrass S, Marquez J, de Zoete R, Rivett DA. Clinical benefits of joint mobilization on ankle sprains: a systematic review and meta-analysis. Archives of physical medicine and rehabilitation. 2018 Jul 1;99(7):1395-412. Link
Gogate N, Satpute K, Hall T. The effectiveness of mobilization with movement on pain, balance and function following acute and sub acute inversion ankle sprain–A randomized, placebo controlled trial. Physical Therapy in Sport. 2020 Dec 23. Link
Nguyen AP, Pitance L, Mahaudens P, Detrembleur C, David Y, Hall T, Hidalgo B. Effects of Mulligan Mobilization with Movement in Subacute Lateral Ankle Sprains: A Pragmatic Randomized Trial. Journal of Manual & Manipulative Therapy. 2021 Feb 28:1-2. Link
Brantingham JW, Cassa TK, Bonnefin D, Pribicevic M, Robb A, Pollard H, Tong V, Korporaal C. Manipulative and multimodal therapy for upper extremity and temporomandibular disorders: a systematic review. Journal of manipulative and physiological therapeutics. 2013 Mar 1;36(3):143-201. Link
Pilar Mansilla-Ferragut, DO, César Fernández-de-las Peñas, DO, PhD, Francisco Alburquerque-Sendi`n, DO, PhD, Joshua A. Cleland, PhD, and Juan José Boscá-Gandi. DO J Manipulative Physiol Ther 2009;32:101-106
Reynolds B, Puentedura EJ, Kolber MJ, Cleland JA. Effectiveness of cervical spine high velocity low amplitude thrust added to behavioral education, soft tissue mobilization, and exercise in individuals with temporomandibular disorder (TMD) with myalgia: A randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy. 2020 Jan 6(0):1-40. Link
Schneider M, Haas M, Glick R, Stevans J, Landsittel D. A comparison of spinal manipulation methods and usual medical care for acute and Sub-acute low back pain: a randomized clinical trial. Spine. 2015 Feb 15;40(4):209. Link
Sarnat RL, Winterstein J. Clinical and cost outcomes of an integrative medicine IPA. Journal of Manipulative and Physiological Therapeutics. 2004 Jun 1;27(5):336-47. Link
Korthals-de Bos IB, Müllner M, Hoving JL, van Tulder MW, Rutten-van Mölken MP, Adèr HJ, de Vet HC, Koes BW, Vondeling H, Bouter LM. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: economic evaluation alongside a randomised controlled trialCommentary: Bootstrapping simplifies appreciation of statistical inferences. Bmj. 2003 Apr 26;326(7395):911-4. Link
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2017 Apr 4;166(7):514-30. Link
FDA. FDA Education Blueprint for Health Care Providers Involved in the Management or Support of Patients with Pain. U.S. Food and Drug Administration. Link
Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. Jama. 2016 Apr 19;315(15):1624-45. Link
United States Bone and Joint Initiative: The Burden of Musculoskeletal Diseases in the United States (BMUS), Third Edition, 2014. Rosemont, IL. Link
Liliedahl RL, Finch MD, Axene DV, Goertz CM. Cost of care for common back pain conditions initiated with chiropractic doctor vs medical doctor/doctor of osteopathy as first physician: experience of one Tennessee-based general health insurer. Journal of manipulative and physiological therapeutics. 2010 Nov 1;33(9):640-3. Link
Houweling TA, Braga AV, Hausheer T, Vogelsang M, Peterson C, Humphreys BK. First-contact care with a medical vs chiropractic provider after consultation with a Swiss telemedicine provider: comparison of outcomes, patient satisfaction, and health care costs in spinal, hip, and shoulder pain patients. Journal of manipulative and physiological therapeutics. 2015 Sep 1;38(7):477-83. Link
Hinkeldey N, Okamoto C, Khan J. Spinal Manipulation and Select Manual Therapies: Current Perspectives. Physical Medicine and Rehabilitation Clinics. 2020 Nov 1;31(4):593-608. Link
Keeney BJ, Fulton-Kehoe D, Turner JA, Wickizer TM, Chan KC, Franklin GM. Early predictors of lumbar spine surgery after occupational back injury: results from a prospective study of workers in Washington State. Spine. 2013 May 15;38(11):953. Link
Elton D. The distribution and analysis of annualized claims data for more than 3.7 million commercial health plan members. Data retrieved from the UnitedHealthcare national commercial claims database, July 1, 2013–June 30, 2014. 2014 Nov.
Lilly DT, Davison MA, Eldridge CM, Singh R, Montgomery EY, Bagley C, Adogwa O. An Assessment of Nonoperative Management Strategies in a Herniated Lumbar Disc Population: Successes Versus Failures. Global Spine Journal. 2020 Jul 7:2192568220936217. Link
Schreijenberg M, Lin CW, Mclachlan AJ, Williams CM, Kamper SJ, Koes BW, Maher CG, Billot L. Paracetamol is ineffective for acute low back pain even for patients who comply with treatment: complier average causal effect analysis of a randomized controlled trial. Pain. 2019 Dec 1;160(12):2848-54. Link
van der Gaag WH, Roelofs PD, Enthoven WT, van Tulder MW, Koes BW. Non‐steroidal anti‐inflammatory drugs for acute low back pain. Cochrane Database of Systematic Reviews. 2020(4). Link
Abdel Shaheed C, Maher CG, Williams KA, McLachlan AJ. Efficacy and tolerability of muscle relaxants for low back pain: systematic review and meta‐analysis. European Journal of Pain. 2017 Feb;21(2):228-37. Link
Ebell MH. Gabapentin and Pregabalin Not Effective for Low Back Pain with or Without Radiculopathy. American family physician. 2019 Mar 15;99(6). Link
Ashworth J, Green DJ, Dunn KM, Jordan KP. Opioid use among low back pain patients in primary care: Is opioid prescription associated with disability at 6-month follow-up?. PAIN®. 2013 Jul 1;154(7):1038-44. Link
NSC. Addressing the Opioid Crisis. National Safety Council. Accessed on 08/20/2021 from https://www.nsc.org/home-safety/safety-topics/opioids
Paulozzi MD, Jones PharmD, et al. Vital Signs: Overdoses of Prescription Opioid Pain Relievers – United State, 1999-2008. Division of Unintentional Injury Prevention, National Center for Injury Prevention and Control, Center for Disease Control and Prevention. 2011:60:5.
Corcoran KL, Bastian LA, Gunderson CG, Steffens C, Brackett A, Lisi AJ. Association between chiropractic use and opioid receipt among patients with spinal pain: a systematic review and meta-analysis. Pain Medicine. 2020 Feb 1;21(2):e139-45. Link
Whedon JM, Toler AW, Kazal LA, Bezdjian S, Goehl JM, Greenstein J. Impact of chiropractic care on use of prescription opioids in patients with spinal pain. Pain Medicine. 2020 Dec 25;21(12):3567-73. Link
Feldman V, Return on investment analysis of Optum offerings — assumes Network/UM/Claims services; Optum Book of Business Analytics 2013.
Paige NM, Miake-Lye IM, Booth MS, Beroes JM, Mardian AS, Dougherty P, Branson R, Tang B, Morton SC, Shekelle PG. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. Jama. 2017 Apr 11;317(14):1451-60. Link
Whedon JM, Mackenzie TA, Phillips RB, Lurie JD. Risk of traumatic injury associated with chiropractic spinal manipulation in Medicare Part B beneficiaries aged 66–99. Spine. 2015 Feb 15;40(4):264. Link
Farah & Farah. Medical Malpractice By State: Exploring Medical Malpractice Across America From 1990 to 2017. Farah & Farah. Link
Martin K. Malpractice Premium Report 2019. Medscape. 2019 Dec. Link
NCMIC Premium Data. Provided via email from Michael Whitmer to Tim Bertelsman on 08/05/2021.
Whedon JM, Bezdjian S, Dennis P, Fischer VA, Russell R. Cost comparison of two approaches to chiropractic care for patients with acute and sub-acute low Back pain care episodes: a cohort study. Chiropractic & manual therapies. 2020 Dec;28(1):1-7. Link
Weeks WB, Leininger B, Whedon JM, Lurie JD, Tosteson TD, Swenson R, O’Malley AJ, Goertz CM. The association between use of chiropractic care and costs of care among older Medicare patients with chronic low back pain and multiple comorbidities. Journal of manipulative and physiological therapeutics. 2016 Feb 1;39(2):63-75. Link
Dagenais S, Haldeman S, Manga P. A systematic review comparing the costs of chiropractic care to other interventions for spine pain in the United States. BMC health services research. 2015 Jun;15(1):1-21. Link
Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. The Spine Journal. 2016 Nov 1;16(11):1292-304. Link
Davis MA, Yakusheva O, Gottlieb DJ, Bynum JP. Regional supply of chiropractic care and visits to primary care physicians for back and neck pain. The Journal of the American Board of Family Medicine. 2015 Jul 1;28(4):481-90. Link
Legorreta AP, Metz RD, Nelson CF, Ray S, Chernicoff HO, DiNubile NA. Comparative analysis of individuals with and without chiropractic coverage: patient characteristics, utilization, and costs. Archives of Internal Medicine. 2004 Oct 11;164(18):1985-92. Link
Roos EM, Herzog W, Block JA, et al. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat Rev Rheumatol. 2011;7:57–63. Link
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, Halabi S, Turner JA, Avins AL, James K, Wald JT, Kallmes DF, Jarvik JG. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. Am J Neuroradiol. 2015 Apr;36(4):811-6. Link
Jarvik JG, Deyo RA. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002 Oct 1;137(7):586–97. Link
Girish G, Lobo LG, Jacobson JA, Morag Y, Miller B, Jamadar DA. Ultrasound of the shoulder: asymptomatic findings in men. American Journal of Roentgenology. 2011 Oct;197(4):W713-9. Link