What is Joint Manipulation?
Reading time: 4 minutes
Joint manipulation does not occur outside the anatomical constraints of a joint. It does, however, occur outside of a joint's physiologic range of motion.
These statements contradict the historically accepted model proposed by Sandoz in 1976. It aligns more closely with the model proposed by Evans and Breen in 2006. The difference between these models may change how you educate your patients and think about joining manipulation. This blog aims to compare the two models and then provide a novel opinion end the end.
What Causes A Joint To Pop?
The COLLAPSE of vapor bubbles
In the 1970s, Sandoz et al. attributed the popping sound to the collapse of vapor cavities released from within the joint synovial fluid. This model was referred to as the cavitation phenomenon. (1)
The CREATION of vapor bubbles
In 2015, an examination of ten metacarpophalangeal joints with real-time magnetic resonance imaging revealed that the "tribonucleation" phenomenon could cause the popping sound. This physical process of manipulation involves a rapid separation of the joint surfaces and subsequent gas cavity formation with an audible release. (2)
How Do Chiropractors Pop Joints?
The Santoz model was the original joint manipulation model resulting in an audible "pop." Most chiropractors have seen this model in their education. It does have a flaw often exposed yet under appreciated in the chiropractic profession. Sandoz proposed that the pop occurs once joint motion exceeds an arbitrary elastic barrier at a joint's anatomical integrity limit. So, the joint must be stretched beyond its normal range of motion and enters a paraphysiologic space. There are two main issues with this model. (3)
To hear a pop, manipulation forces must be great enough to pull joint surfaces away from each other. Distractive forces overcome the pressure of the synovial fluid to achieve joint cavitation. Is it the collapse of the bubbles, or creation of the vapor bubble? It is likely a mixture of both.
Stretching a joint beyond its anatomic limits would result in injury to tissue. If joint manipulation were the result of stretching tissue past its anatomical limit, it would be a sprain or strain to the musculoskeletal structures. Joint manipulation, when performed appropriately, does so without injury to surrounding tissue.
So, how do we pull joints apart without exceeding the anatomic limits of the joint? Evans and Breen purposed a model of joint manipulation that has several key differences: (2,4)
The para-physiological space is not the range of motion that exceeds the anatomic limits. Instead, it is a space created within a normal capsular range of motion. Imagine pulling your finger. If you pull hard enough, you may hear a popping sound. As the joint volume increases, the synovial fluid's pressure decreases, and eventually, a cavitation/tribonucleation event occurs. Keep in mind, throughout that finger range of motion, you never exceed the anatomic limits of that joint yet still hear a pop.
Also, it is essential to note that joint manipulation is easiest with a joint in a neutral position—not at the end range. The take-home point is that the manipulation setup and preload phase is about reducing soft and hard tissue limiting factors before delivering a high-velocity low amplitude thrust and not taking a joint to end range. I would argue, if the joint is at the end range within this model, it should take more force to hear a pop. Capsular stiffness may limit the ability of the joint surfaces to gap.
What Limits Joint Range of Motion?
A number of factors can limit a joint's range of motion (ROM). Every joint has an anatomical limit to how far it can move. Factors that restrict this anatomical range of motion include:
Muscular tightness or imbalance: When specific muscles are tight or weaker than others, they can prevent a joint from moving through its full range of motion. For example, tight hip flexors can limit the extension and external rotation of the hip joint.
Joint stiffness: As we age, joints tend to become stiffer and less mobile, limiting their range of motion. Arthritis, injury, and other conditions can also cause joint stiffness. Increased joint stiffness and contracture are common results of repetitive postural stresses imparted on capsules. (5)
Soft tissue restrictions: Adhesions, scar tissue, and other soft tissue restrictions can limit joint movement. Adhesions within or between fascia are a known factor limiting normal joint mechanics.
Bone or cartilage abnormalities: Certain bone or cartilage abnormalities, such as bone spurs, can also limit a joint's range of motion.
Pain or discomfort: Pain or discomfort in a joint can cause a person to avoid moving it through its full range of motion, leading to stiffness and further limitations in ROM.
What If The Joint Doesn’t Pop?
Joint manipulation has multiple utilities: musculoskeletal, chemical, and neurophysiological. The audible (cavitation/tribonucleation) event may not be necessary for therapeutic benefit. Multiple studies have shown no evidence of improved pain outcomes associated with or without an audible pop. (6) However, most patients expect to hear the sound and associate it with a successful manipulation. (7) Here are three tips when addressing this topic with a patient.
When cavitation occurs, it is not the treatment. The therapeutic benefit is reducing all factors that have limited the joint's range of motion. The pop signifies the joint has a full available range of motion in the direction of manipulation for that segment.
Some joints already have ample range of motion. Have you ever noticed that after manipulating a joint, it will not pop again for an extended period? Joints that have a full range of motion or continuously use a full range of motion will not pop as easily. For this reason, hypermobile and very active people are often the most difficult to manipulate.
Sometimes joint motion is limited by soft or hard tissue factors. For example, if the patient is nervous and guarding against the provider, it may be difficult for the joint to gap. Also, joints with degeneration may have a limited range of motion, reducing joint surfaces' ability to separate. The utility of joint manipulation is inversely proportional to the joint's degeneration.
As an evidence-based chiropractor, you're probably aware of the complexities of diagnosing and treating musculoskeletal conditions. In this context, it's essential to recognize that restricted joint range of motion can serve as both a clinical sign and, in some cases, a diagnosis.
The brilliance of chiropractors lies in their ability to identify the factors that are limiting joint motion. By doing so, we can determine what combination of manipulation, manual therapy, exercise, and education will be effective in helping each patient recover.
The identification and correction of restricted joint range of motion is a diagnostic factor crucial to effective patient care.
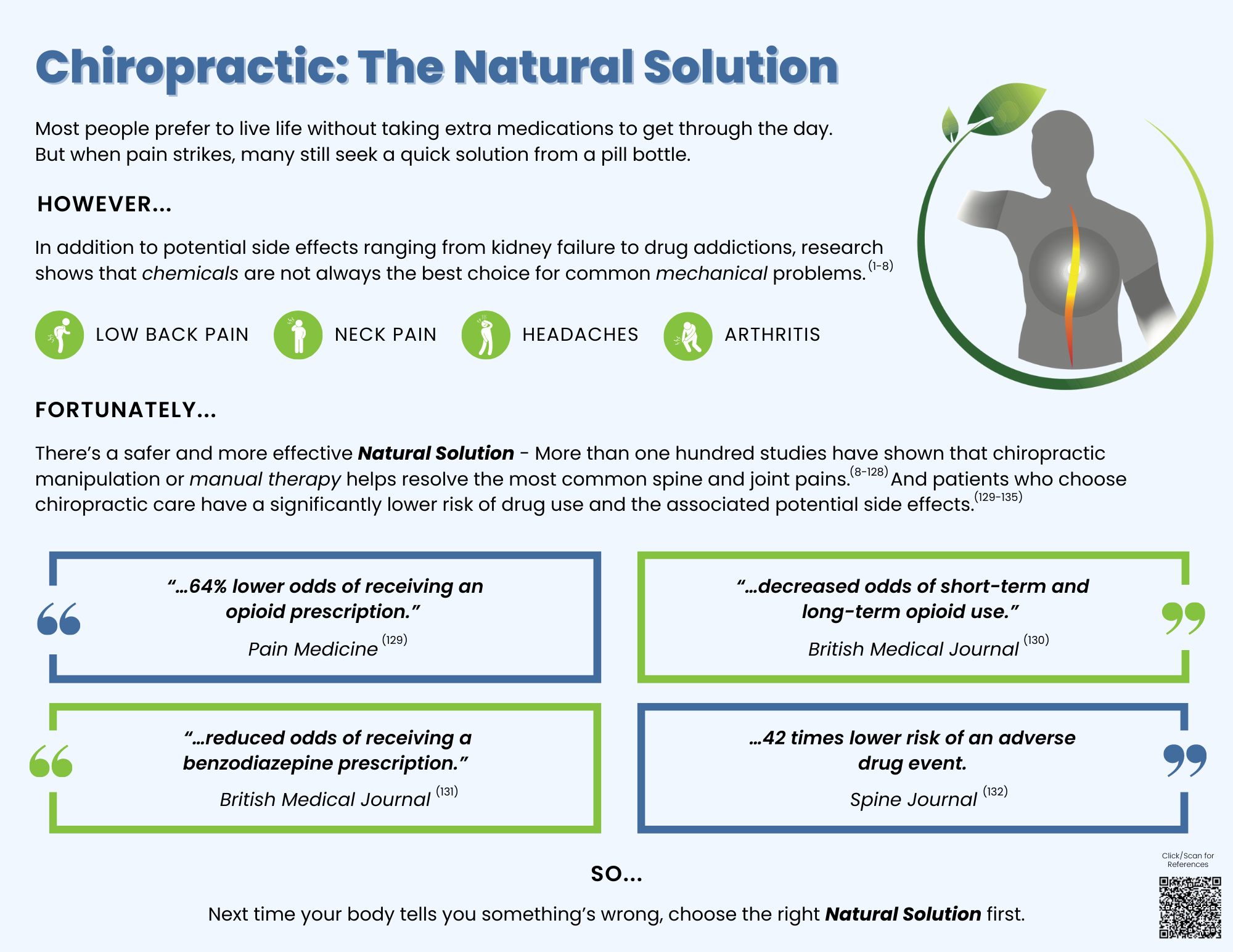
ChiroUp subscribers: Download our new, customizable Natural Solution patient infographic in the forms library by searching “Natural Solution” to share the facts about the effectiveness and safety of chiropractic spinal manipulation.
Not a subscriber? Get FREE 14-day access to ChiroUp now to get more patient materials like this!
-
Sandoz R. Some physical mechanisms and effects of spinal adjustments. Ann Swiss Chiropr Assoc. 1976;6:91–141.
Kawchuk GN, Fryer J, Jaremko JL, Zeng H, Rowe L, Thompson R. Real-time visualization of joint cavitation. PLoS ONE. 2015;10(4): e0119470.
Evans DW. Why is the prevailing model of joint manipulation (still) incorrect? Chiropractic & manual therapies. 2022 Dec 9;30(1):51.
Evans DW, Breen AC. A biomechanical model for mechanically efficient cavitation production during spinal manipulation: prethrust position and the neutral zone. J Manip Physiol Ther. 2006;29(1):72–82.
Dashottar, A., & Borstad, J. (2012). Posterior glenohumeral joint capsule contracture. Shoulder & elbow, 4(4).
Moorman, A.C., Newell, D. Impact of audible pops associated with spinal manipulation on perceived pain: a systematic review. Chiropr Man Therap 30, 42 (2022).
Fernández-de-las-Penas C, Testa M. Patient Concerns and Beliefs Related to Audible Popping Sound and the Effectiveness of Manipulation: Findings From an Online Survey.