7 Essential Cervicogenic Vertigo Facts Every DC Must Own
Reading time: 5 minutes
Neck pain and vertigo are common co-morbidities. One recent study of 2,361 patients concluded that up to 40% of neck pain patients will experience cervicogenic dizziness. (96). Fortunately, significant research, including the 2021 ChiroUp COPS synopsis of 631,970 diagnoses, found that the combination of neck pain and vertigo is one of the ten most responsive complaints to chiropractic care.
So, to ensure you’re the go-to doc for patients with vertigo and neck pain, this blog will review seven essential cervical vertigo facts.
1. What Causes Cervical Vertigo?
Short answer: A mismatch of sensory information that temporarily confuses the brain.
Deeper dive
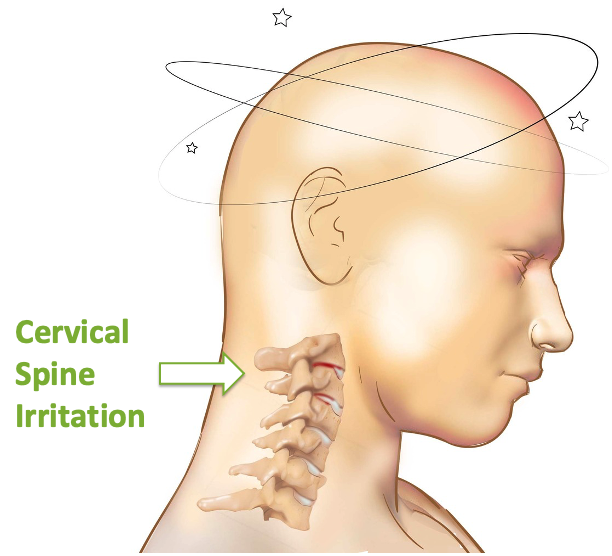
Although the exact mechanism of cervical dizziness is debatable, most researchers ascribe to an altered "mechanoreceptive" theory. The upper cervical (C0-3) facet joints are highly innervated, supplying up to 50% of all cervical proprioceptive input. (11,83) The cervical spine muscles, particularly the suboccipital muscles, are extensively supplied with muscle spindles providing additional contributions. (12,81,82)
Patients with neck pain and vertigo frequently exhibit muscle hypertonicity, limited upper cervical ROM, and joint position errors. (84) The abnormal stimulation of the articular capsule or muscular spindle mechanical receptors provides conflicting input with visual and vestibular afferents. This sensory mismatch between visual, vestibular, and cervical mechanoreceptive input "confuses" the brain into a temporary state of dizziness. (11,13-18,78)
2. What Are the Most Common Cervicogenic Dizziness Symptoms?
Short answer: Neck discomfort and unsteadiness.
Deeper Dive:
Cervicogenic vertigo is suggested by a history of dizziness associated with cervical movement and likely concurrent neck discomfort. (32,33) Cervical vertigo symptoms include light-headedness, floating, unsteadiness, or general imbalance, but rarely true “spinning” vertigo. (27,97) A sensation of “spinning” (i.e., true rotary vertigo) usually suggests a non-cervicogenic origin, possibly Benign Paroxysmal Positional Vertigo (BPPV). (21) Symptoms of cervical vertigo are generally episodic, provoked by movement, and eased by maintaining a stable position.
3. What Are the Key Cervicogenic Vertigo Assessment Findings?
Short answer: Upper cervical tenderness, hypertonicity, and restriction.
Deeper Dive
Findings consistent with a diagnosis of cervicogenic vertigo include loss of cervical range of motion, upper cervical tenderness, and upper cervical segmental joint restriction. Deep palpation of the suboccipital region may reproduce vertigo in some patients. (40) Clinicians often note hypertonicity in the suboccipital, paracervical, trapezius, SCM, and pectoral muscles. A cyclic pattern of dysfunction has been identified between altered cervical proprioception and hypertonicity in the SCM and upper trapezius that may fuel cervicogenic vertigo. (21,38,42)
4. What Is The Difference Between BPPV and Cervical Vertigo?
Short answer: Very subtle symptomatic differences, plus cervical involvement.
Deeper Dive
Benign Paroxysmal Positional Vertigo, or BPPV, is responsible for 17-42% of all dizziness presentations. BPPV occurs when small otoliths dislodge from the utricle and move into one of the semicircular canals, thereby sending conflicting balance information to the brain. (3,37) Symptoms of cervicogenic dizziness can closely mirror BPPV. However, BPPV patients typically report a “spinning vertigo” sensation, whereas BPPV is more likely perceived as “drunkenness” or “light-headedness.” (97)
Another significant differentiator is that isolated cervicogenic vertigo is nearly always accompanied by loss of cervical range of motion, upper cervical tenderness, and upper cervical segmental joint restriction. (85,86) However, clinicians should remember that cervicogenic vertigo and BPPV (or other etiologies) can co-exist.
Bonus: Check out this recent ChiroUp BPPV blog for a complete synopsis, including the best tests and treatments for BPPV.
5. What’s The Best Cervical Dizziness Test?
Short answer: The cervical torsion test.
Deeper Dive
One complicating factor in the differentiation of cervicogenic vertigo versus BPPV is that most provocative movements simultaneously stimulate cervical spine proprioceptors and the vestibular apparatus. According to an October 2022 Journal of Clinical Medicine review, the cervical torsion test is the best method for overcoming this challenge and diagnosing cervicogenic vertigo. (95)
The Head-fixed/body-turn test (aka Neck torsion test or Fitz Ritson test) aims to isolate cervical mechanoreceptors without stimulating the vestibular apparatus. (21,41) The neck torsion test is performed with the patient rotating their body on an exam stool while the clinician stabilizes their head, thereby minimizing vestibular input. Reproduction of dizziness or nystagmus when the head is stable suggests a cervical component. (42-44)
Bonus: ChiroUp subscribers can review the Cervical Torsion Test video tutorial here.
6. What’s The Best Cervicogenic Dizziness Treatment?
Short answer: Spinal manipulation and manual therapy (after other etiologies have been ruled out).
Deeper Dive
Cervical dizziness is quite amenable to manual therapy. (16,21,29, 47-49,54,57) Since cervicogenic vertigo, by definition, results from upper cervical dysfunction, spinal manipulation is a cornerstone of treatment. Several studies have demonstrated the effectiveness of spinal manipulation for cervical vertigo. (11,59,60,87-89,92,93)
One of the world’s foremost musculoskeletal experts, Karel Lewit, M.D., states, “In no field is manipulation more effective than in the treatment of disturbances of equilibrium.” (61) Fitz-Ritson demonstrated a 90.2 success rate when utilizing manipulation for the treatment of post-traumatic cervical vertigo. (17)
Because the condition is multifactorial in origin, successful cervical vertigo treatment requires a multi-faceted approach. Treatment for cervical vertigo must address associated soft tissue components. Myofascial release and stretching may be needed in the suboccipital, SCM, upper trapezius, levator, and pectoral muscles. Postural correction may be necessary for upper crossed syndrome, and breathing exercises are appropriate for those with dysfunctional respiration. Clinicians should be particularly mindful to assess and correct for weakness in the deep neck flexor muscles (i.e., longus colli and longus capitis).
Bonus: ChiroUp subscribers can review the complete cervicogenic vertigo treatment protocol, including the top cervical vertigo exercises and soft tissue techniques.
7. What Other Causes of Dizziness Do Clinicians Need to Consider?
Short answer: Lots!
Deeper dive:
Cervicogenic dizziness is a diagnosis of exclusion, as there is no pathognomonic test to confirm its presence. (34-35) Clinicians should be particularly astute and unhurried when evaluating vertigo. The common co-existence of vertigo and upper cervical discomfort has the potential to lull clinicians into a dangerous state of diagnostic complacency. Falsely assuming that someone with concurrent dizziness and neck pain is suffering from cervicogenic vertigo, without ruling out other potentially threatening causes of dizziness, could end unfavorably.
Dizziness affects 15-20% of the population each year. (98) Fortunately, evidence-based chiropractors are well-equipped to manage the most common benign culprits and appropriately refer the more threatening causes.
Bonus: Be the GO-TO Doc! Watch our latest on-demand webinar, Managing the Dizzy Patient, for an informative discussion on evaluating and treating the most common causes of vertigo. This webinar will include practical skills for managing cervicogenic vertigo and BPPV, plus valuable tips for identifying the more threatening presentations. And as an added incentive, we’ll send your our Vertigo toolkit, including the following:
Differential Diagnosis of Dizziness 1-page synopsis
CAD Clinical Pearls infographic
Epley Maneuver quick reference card
Safety of SMT infographic and blog (Lay education)
-
1. Lalwani AK. Vertigo dysequilibrium and imbalance with aging. In: Jackler RK, Brackmann DE, editors. Neurotology. St. Louis: Mosby; 1994. p. 527-34.
2. Colledge NR, Barr-Hamilton RM, Lewis SJ, Sellar RJ, Wilson JA. Evaluation of investigations to diagnose the cause of dizziness in elderly people: a community based controlled study. Bmj. 1996 Sep 28;313(7060):788-92. Link
3. Albernaz PLM, Cruz NA, Ganaça MM. As doenças vestibulares periféricas e centrais: classificação, diagnóstico e tratamento. Rev Bras Otorinolaring 1968:541-8.
4. de Jong PT, De Jong JV, Cohen B, Jongkees LB. Ataxia and nystagmus induced by injection of local anesthetics in the neck. Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society. 1977 Mar;1(3):240-6. Link
5. Abrahams VC, Falchetto S. Hind leg ataxia of cervical origin and cervico-lumbar spinal interactions with a supratentorial pathway. The Journal of physiology. 1969 Aug;203(2):435. Link
6. Fitz-Ritson D. Neuroanatomy and neurophysiology of the upper cervical spine. The Upper Cervical Syndrome: Chiropractic Diagnosis and Treatment. Baltimore: Williams and Wilkens. 1988:48-85.
7. Guyton AC. Textbook of Medical Physiology. 7th ed. Philadelphia: Lea and Febiger, 1989.
9. RyanMS,CopeS.Cervicalvertigo.Lancet.1955;2:1355- 1358.
10. FurmanJM,CassSP. BalanceDisorders: A Case-StudyAp- proach. Philadelphia, Pa: FA Davis; 1996.
11. Hulse M. Disequelibrium caused by a functional disturbance of the upper cervical spine, clinical aspects and differential diagnosis. Manual Medicine. 1983;1(1):18-23.
12. Cooper S, Daniel PM. Muscle spindles in man; their morphology in the lumbricals and the deep muscles of the neck. Brain. 1963 Sep 1;86(3):563-86. Link
13. Telian SA, Shepard NT. Update on vestibular rehabilitation therapy. Otolaryngologic Clinics of North America. 1996 Apr;29(2):359-71. Link
14. Wyke B. Neurology of the cervical spinal joints. Physiotherapy. 1979 Mar;65(3):72-6.
15. Baloh RW. Dizziness, hearing loss, and tinnitus: the essentials of neurotology. FA Davis Co; 1984.
16. Biesinger E. Vertigo caused by disorders of the cervical vertebral column. InRecent Concepts in ORL 1988 (Vol. 39, pp. 44-51). Karger Publishers. Link
17. Fitz-Ritson D. Assessment of cervicogenic vertigo. Journal of manipulative and physiological therapeutics. 1991;14(3):193-8. Link
18. Zuo J, Han J, Qiu S, Luan F, Zhu X, Gao H, Chen A. Neural reflex pathway between cervical spinal and sympathetic ganglia in rabbits: implication for pathogenesis of cervical vertigo. The Spine Journal. 2014 Jun 1;14(6):1005-9. Link
19. Brandt T, Bronstein AM. Cervical vertigo J Neurol Neurosurg Psychiatry 2001;71:8-12
20. Eduardo S. B. Bracher, DC, MD,a Clemente I. R. Almeida, MD,b Roberta R. Almeida, MD,b,c André C. Duprat, MD,b and Cheri B. B. Bracher, DCa A Combined Approach for the Treatment of Cervical Vertigo J Manipulative Physiol Ther 2000;23:96-100).
21. Wrisley DM, Sparto PJ, Whitney SL, Furman JM. Cervicogenic dizziness: a review of diagnosis and treatment. Journal of Orthopaedic & Sports Physical Therapy. 2000 Dec;30(12):755-66. Link
22. Oostendorp RA, VanEupen AA, VanErp JM, Elvers HW. Dizziness following whiplash injury: a neuro-otological study in manual therapy practice and therapeutic implication. Journal of Manual & Manipulative Therapy. 1999 Jul 1;7(3):123-30. Link
23. Rubin W. Whiplash with vestibular involvement. Arch Otolaryngol. 1973;97:85-87.
24. Spitzer WO. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining" whiplash" and its management. Spine. 1995;20:1S-73S.
25. Endo K, Ichimaru K, Komagata M, Yamamoto K. Cervical vertigo and dizziness after whiplash injury. European Spine Journal. 2006 Jun 1;15(6):886-90. Link
27. Takasaki H, Johnston V, Treleaven J, Pereira M, Jull G. Driving with a chronic whiplash-associated disorder: a review of patients' perspectives. Archives of physical medicine and rehabilitation. 2011 Jan 1;92(1):106-10. Link
28. Spitzer WO. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: redefining" whiplash" and its management. Spine. 1995;20:1S-73S.
29. BrownJJ. Cervical contributions to balance: cervical vertigo. In: Berthoz A, Vidal PP, Graf W, eds. The Head Neck Sensory Motor System. New York, NY: Oxford University Press; 1992:644-647.
30. Basmajian JV. Basis for autonomic regulation. In: Basmajian J, editor. Biofeedback principle and practice for clinicians. Baltimore:William & Wilkins; 1989. p. 37-48.
31. Hatch JP. Headache. In: Gatcher RJ, Blanchard EB, editors. Psychophysiologycal disorders. Washington, DC: American Psychologycal Association; 1994. p. 111-49.
32. Ojala M, Palo J. The aetiology of dizziness and how to examine a dizzy patient. Annals of medicine. 1991 Jan 1;23(3):225-30. Link
33. Stenger HH. Análisis del vertigo; exploración del nystagmo espontáneo y del provocado. Tratado de otorrinolaringologia. Barcelona: Editorial Cientifico Médica. 1969:603-46.
34. Huijbregts P, Vidal P. Dizziness in orthopaedic physical therapy practice: Classification and pathophysiology. Journal of Manual & Manipulative Therapy. 2004 Oct 1;12(4):199-214. Link
35. Furman JM, Cass SP. Balance disorders: a case-study approach. Oxford University Press, USA; 1996 Jun 15.
36. Côté P, Mior SA, Fitz-Ritson D. Cervicogenic vertigo: a report of three cases. The Journal of the Canadian Chiropractic Association. 1991 Jun;35(2):89. Link
37. Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, Chalian AA, Desmond AL, Earll JM, Fife TD, Fuller DC. Clinical practice guideline: benign paroxysmal positional vertigo. Otolaryngology--head and neck surgery. 2008 Nov;139(5_suppl):47-81. Link
39. Weiner HL, Levitt LP. Neurology for the house officer. Baltimore: Williams & Wilkins; 1978 Sep 20.
40. Norre M, Stevens A. Le nystagmus cervical et les troubles fonctionnels de la colonne cervicale. Acta Oto-Rhino-Larynologica Belgica. 1976;30.
41. Phillipszoon AJ. Neck torsion nystagmus. Pract Oto-Rhi- no-Laryngologist. 1963;25:339-344.
42. Huijbregts P, Vidal P. Dizziness in orthopaedic physical therapy practice: Classification and pathophysiology. Journal of Manual & Manipulative Therapy. 2004 Oct 1;12(4):199-214. Link
43. Norre ME, Stevens A. Cervical vertigo. Acta Oto-Rhino-Larynologica Belgica 1987; 41(3):436-52.
44. Fitz-Ritson D. Assessment of cervicogenic vertigo. J Manipulative Physiol Ther. 1991 Mar-Apr;14(3):193-8.
45. Tjell C, Rosenhall U. Smooth pursuit neck torsion test: a specific test for cervical dizziness. The American journal of otology. 1998 Jan;19(1):76-81. Link
47. Galm R, Rittmeister M, Schmitt E. Vertigo in patients with cervical spine dysfunction. European Spine Journal. 1998 Feb 1;7(1):55-8. Link
48. Karlberg M, Magnusson M, Eva-Maj M, Agneta M, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Archives of physical medicine and rehabilitation. 1996 Sep 1;77(9):874-82. Link
49. Wing LW, Hargrave-Wilson W. Cervical vertigo. Aust N Z J Surg 1974;44:275–277.
54. Galm R, Rittmeister M, Schmitt E. Vertigo in patients with cervical spine dysfunction. European Spine Journal. 1998 Feb 1;7(1):55-8. Link
57. Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Manual therapy. 2005 Feb 1;10(1):4-13. Link
58. Oostendorp RA, VanEupen AA, VanErp JM, Elvers HW. Dizziness following whiplash injury: a neuro-otological study in manual therapy practice and therapeutic implication. Journal of Manual & Manipulative Therapy. 1999 Jul 1;7(3):123-30. Link
59. Brunarski D. Autonomic nervous system disturbances of cervical origin including disorders of equilibrium. Upper Cervical Syndrome. Baltimore: Williams and Wilkins. 1988:189-93.
60. Fitz-Ritson D. The chiropractic management and rehabilitation of cervical trauma. Journal of manipulative and physiological therapeutics. 1990 Jan;13(1):17-25. Link
61. Lewit K. Disturbed balance due to lesions of the cranio-cervical junction. J Orthop Med 1998; 3:58-61.
62. Reid SA, Rivett DA, Katekar MG, Callister R. Sustained natural apophyseal glides (SNAGs) are an effective treatment for cervicogenic dizziness. Manual therapy. 2008 Aug 1;13(4):357-66. Link
63. Bourgeois PM, Dehaene I. Benign paroxysmal positional vertigo. Acta Neurol Belg 1988; 88:65-74.
64. Norré ME, Beckers AM. Vestibular habituation training: specificity of adequate exercise. Archives of Otolaryngology–Head & Neck Surgery. 1988 Aug 1;114(8):883-6. Link
68. Karlberg M, Magnusson M, Eva-Maj M, Agneta M, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Archives of physical medicine and rehabilitation. 1996 Sep 1;77(9):874-82. Link
69. Dal T, Özlüo?lu LN, Ergin NT. The canalith repositioning maneuver in patients with benign positional vertigo. European archives of oto-rhino-laryngology. 2000 Apr 1;257(3):133-6. Link
70. Herdman SJ, Tusa RJ, Zee DS, Proctor LR, Mattox DE. Single treatment approaches to benign paroxysmal positional vertigo. Archives of Otolaryngology–Head & Neck Surgery. 1993 Apr 1;119(4):450-4. Link
71. Wolf JS, Boyev KP, Manokey BJ, Mattox DE. Success of the modified Epley maneuver in treating benign paroxysmal positional vertigo. The Laryngoscope. 1999 Jun;109(6):900-3. Link
72. Wolf M, Hertanu T, Novikov I, Kronenberg J. Epley’s manoeuvre for benign paroxysmal positional vertigo: a prospective study 1. Clinical Otolaryngology & Allied Sciences. 1999 Feb;24(1):43-6. Link
74. Macias JD, Ellensohn A, Massingale S, Gerkin R. Vibration with the canalith repositioning maneuver: a prospective randomized study to determine efficacy. The Laryngoscope. 2004 Jun;114(6):1011-4. Link
75. Hain TC, Helminski JO, Reis IL, Uddin MK. Vibration does not improve results of the canalith repositioning procedure. Archives of Otolaryngology–Head & Neck Surgery. 2000 May 1;126(5):617-22. Link
76. Brandt T, Daroff RB. Physical therapy for benign paroxysmal positional vertigo. Archives of Otolaryngology. 1980 Aug 1;106(8):484-5. Link
77. Bronstein AM, Hood JD. The cervico-ocular reflex in normal subjects and patients with absent vestibular function. Brain research. 1986 May 14;373(1-2):399-408. Link
78. Reid SA, Callister R, Snodgrass SJ, Katekar MG, Rivett DA. Manual therapy for cervicogenic dizziness: Long-term outcomes of a randomised trial. Manual Therapy 20, 2015, 148-56.
79. Peng B. Cervical vertigo: historical reviews and advances. World neurosurgery. 2018 Jan 1;109:347-50. Link
80. Jaroshevskyi OA, Payenok OS, Logvinenko AV. Evalution of the effectiveness of multimodal approach to the management of cervical vertigo. Wiadomosci lekarskie (Warsaw, Poland: 1960). 2017;70(3 pt 2):571-3. Link
81. Pettorossi VE, Schieppati M. Neck proprioception shapes body orientation and perception of motion. Frontiers in human neuroscience. 2014 Nov 4;8:895. Link
82. Chu EC, Chin WL, Bhaumik A. Cervicogenic dizziness. Oxford Medical Case Reports. 2019 Dec 9;2019(11):476-8. Link
83. McLain RF. Mechanoreceptor endings in human cervical facet joints. Spine. 1994 Mar;19(5):495-501.
84. Micarelli A, Viziano A, Carlino P, Granito I, Micarelli RX, Alessandrini M. Reciprocal roles of joint position error, visual dependency and subjective perception in cervicogenic dizziness. Somatosensory & Motor Research. 2020 Aug 7:1-9. Link
85. Wu X, Wang X, Zhang G, Guo Z, Wang Y, Wang R, Xiang H, Chen B. Histologic Observation and Significance of Sympathetic Nerve Fiber Distribution on Human Cervical Ligamentum Flavum. Orthopaedic Surgery. Link
86. Carrasco-Uribarren A, Rodriguez-Sanz J, López-de-Celis C, Pérez-Guillen S, Tricás-Moreno JM, Cabanillas-Barea S. Short-term effects of the traction-manipulation protocol in dizziness intensity and disability in cervicogenic dizziness: a randomized controlled trial. Disability and Rehabilitation. 2021 Jan 7:1-9. Link
87. Reid SA, Rivett DA. Manual therapy treatment of cervicogenic dizziness: a systematic review. Manual therapy. 2005 Feb 1;10(1):4-13. Link
88. Yaseen K, Hendrick P, Ismail A, Felemban M, Alshehri MA. The effectiveness of manual therapy in treating cervicogenic dizziness: a systematic review. Journal of physical therapy science. 2018;30(1):96-102. Link
89. Jin X, Du HG, Qiao ZK, Huang Q, Chen WJ. The efficiency and safety of manual therapy for cervicogenic cephalic syndrome (CCS): A systematic review and meta-analysis. Medicine. 2021 Feb 26;100(8). Link
90. Micarelli A, Viziano A, Granito I, Carlino P, Micarelli RX, Augimeri I, Alessandrini M. Postural and clinical outcomes of sustained natural apophyseal glides treatment in cervicogenic dizziness patients: A randomised controlled trial. Clinical Rehabilitation. 2021 Apr 26:02692155211012413. Link
91. De Vestel C, Vereeck L, Van Rompaey V, Reid SA, De Hertogh W. Clinical characteristics and diagnostic aspects of cervicogenic dizziness in patients with chronic dizziness: A cross-sectional study. Musculoskeletal Science and Practice. 2022 Mar 26:102559. Link
92. De Vestel C, Vereeck L, Reid SA, Van Rompaey V, Lemmens J, De Hertogh W. Systematic review and meta-analysis of the therapeutic management of patients with cervicogenic dizziness. Journal of Manual & Manipulative Therapy. 2022 Apr 7:1-1. Link
93. Carrasco-Uribarren A, Pardos-Aguilella P, Pérez-Guillén S, López-de-Celis C, Rodríguez-Sanz J, Cabanillas-Barea S. Combination of Two Manipulative Techniques for the Treatment of Cervicogenic Dizziness: A Randomized Controlled Trial. Life. 2022 Jul;12(7):1023. Link
94. Cardoso R, Seixas A, Rodrigues S, Moreira-Silva I, Ventura N, Azevedo J, Monsignori F. The effectiveness of Sustained Natural Apophyseal Glide on Flexion Rotation Test, pain intensity, and functionality in subjects with Cervicogenic Headache: A Systematic Review of Randomized Trials. Archives of physiotherapy. 2022 Dec;12(1):1-0. Link
95. Li Y, Yang L, Dai C, Peng B. Proprioceptive Cervicogenic Dizziness: A Narrative Review of Pathogenesis, Diagnosis, and Treatment. Journal of Clinical Medicine. 2022 Oct 26;11(21):6293. Link
96. Vural M, Karan A, Gezer İA, Çalışkan A, Atar S, Aydın FY, Benlidayı İC, Gökşen A, Doğan ŞK, Karacan G, Erdem R. Prevalence, etiology, and biopsychosocial risk factors of cervicogenic dizziness in patients with neck pain: A multi-center, cross-sectional study. Turkish Journal of Physical Medicine and Rehabilitation. 2021 Dec;67(4):399. Link
97. 1. Knapstad MK, Nordahl SH, Goplen FK. Clinical characteristics in patients with cervicogenic dizziness: A systematic review. Health science reports. 2019 Sep;2(9):e134. Link
98. Neuhauser HK. The epidemiology of dizziness and vertigo. Handb Clin Neurol. 2016;137:67-82. doi: 10.1016/B978-0-444-63437-5.00005-4. Link