Top 5 Tips For Resolving Patellar Tendinopathy
Reading time: 6 minutes
Here are 5 evidence-based tips for recognizing and treating tendinopathies. Today’s blog will focus on Patellar Tendinopathy (aka Jumper’s Knee), but you can apply these principles to other tendonous injuries. An evidence-based chiropractor should manage these cases due to our multimodal approach.
If you have patients with knee pain that respond to your initial therapy, but fail to resolve completely, be sure to read tip 3!
1. Recognizing Patellar Tendinopathy Requires You, Not Advanced Imaging.
There are three common symptoms associated with all tendon injuries. (1)
Pain with movement
Focal tendon tenderness
Decreased strength
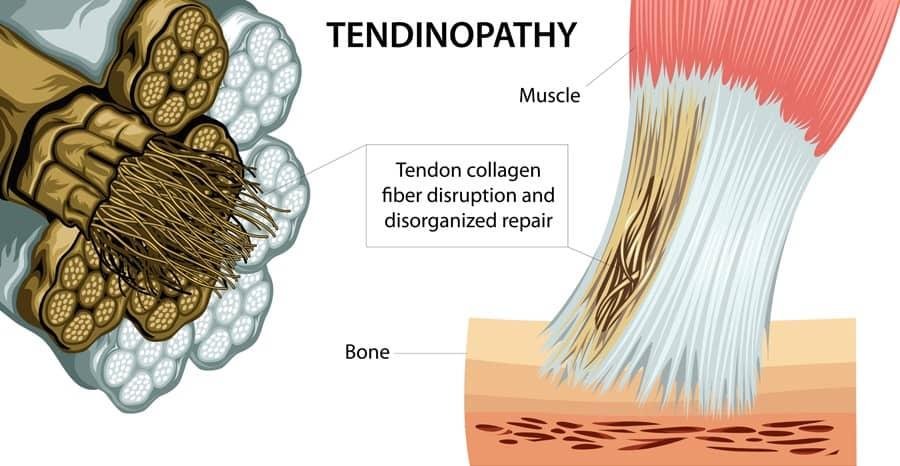
A complete examination and history can tease these three symptoms out within minutes. Tendinopathy is often not visualized at a macroscopic level and, therefore, unnoticed upon advanced imaging. However, microscopically, tendons degenerate from disruption of normal tissue due to repetitive or static loading. Suppose patients do not change their activities or postures. In that case, the tissue will continue degenerating due to a failed healing process—resulting in a painful and weaker tissue. Newly formed collagen is less organized and contains differing ratios of proteoglycans and glycosaminoglycans, and neovascularization. (2)
2. Recognize Patellar Tendinopathy With The Decline Squat Test
Two-thirds of patients present with pain in the characteristic inferior patellar location, but approximately 10% of patellar tendinopathy patients report pain over the tibial tuberosity. (3) Clinicians should be observant for pain or swelling over the tibial tuberosity in skeletally immature athletes, as this likely represents Osgood Schlatter's Disease.
Use the decline squat test to reproduce the patient’s chief complaint. Remember, patients may be apprehensive about completing this test due to pain. Tip: Keep a stable support near the patient to ease their fear of falling to perform the test appropriately.
The patient stands on the affected leg on a 25-degree decline surface and squats. Reproduction of pain suggests irritation to the knee extensor mechanism, especially patellar tendonitis. Clinicians should record the patient's knee flexion angle at the onset of pain and peak intensity during this maneuver to document and monitor progress.
3. Treating Patellar Tendinopathy Requires A Multimodal Approach
If we know what causes tendon injury and how to recognize it, why is it so hard to manage these patients? Some healthcare providers fail to provide these three aspects of care that make all the difference.
Stop the offending activity.
Stopping painful movements sounds like a straightforward treatment strategy, but it is the hardest. Modifying the habits of patients is challenging. Have you ever tried to change someone's posture or told someone to eat healthier… And they did? Habits are hard to form and hard the break!
Consider using infographics and condition reports from ChiroUp to teach patients about their condition and the importance of allowing the tissue to heal correctly. An educated patient is a compliant patient. ChiroUp has already created the condition reports for each diagnosis, but you should also consider delivering the proper infographic. By allowing patients to understand their condition well, you empower them to make educated decisions about their diagnosis.
Teach the patient to be patient during the healing process.
Tendon repair after an injury is slow and begins with inflammation. Within days after a tendon sprain, cell migration and proliferation occur. Remodeling newly formed type 1 collagen does not retain the uninjured tendon's chemical and mechanical properties. Disorganized collagen and scar tissue formation results in newly healed tendons that yield 2/3 less strength than an un-injured tendon. (2) Rushed return to activity only compounds the failed healing process.
For example, youth athletes require better education on how to heal instead of how to enhance performance. Here is an infographic you can use to educate patients about pitching rest time.
Athletes who repetitively injured their tendons without providing ample time to recover yield BIGGER yet weaker tendons. Cushman et al. 2021 finding support the notion that these tendons are beginning the degenerative process well before a pain-limiting injury. They found: "Structural changes in asymptomatic tendons were found in almost 25% of runners. Presence of structural changes was associated with increased development of Achilles and patellar tendon pain within one year." (4)
Progressively load the tissue.
There is hope for these patients. Earp et al. (2022) published a paper stating that: "Moderate loading seems to be sufficient to fully elicit the patellar tendon hyperemic response often attributed to stimulate tendon healing." (5) Tendon loading isn't always hopping on one foot 1 week after and patellar tendon injury. Loading is any movement, stretch, or strengthening, that provides mechanical stress to the tissue.
What exercises should I give my patients with Patellar Tendinopathy?
Both isometric and dynamic loading should have their place in your rehab of these patients. Steffen et al. found that different types of loading result "in different cellular responses within a tendon." Both types of loading are needed to effect proper healing of injured collagen. (6) Your ChiroUp condition report will automatically provide the best exercises for your patients from day 1!
Begin standing downhill on a 25-degree slant board. Very slowly, squat with only the affected knee to 60 degrees at a count of four seconds. Keep your weight on your heel, and do not allow your knee to move forward over the top of your feet during any part of this exercise. You will probably need to extend your arms forward for balance. Use your unaffected leg to return to a standing position. Mild pain is acceptable during this exercise. Stop if the pain grows. Increased resistance may be added by wearing a weighted backpack or holding hand weights. Perform as directed.
Don't think about should I stretch or strengthen first. Both are loading injured tissue. Mechanical forces are necessary for the repair process after tendon injury. Mechanical loading stimulates tendon healing! The exact opposite is equally as important: immobilization is detrimental to the healing process for tendon injuries. (7)
"...eccentric loading with or without adjuncts should remain the first-line treatment for all individuals with patellar tendinopathy." (8)
4. Pain With Rehab Is Not A Stop Sign 🛑 It Is A Gauge 🧭
Most patients think pain is a reason to stop their rehab program. Our responsibility is to inform the patient of the importance of progressive tissue loading in their care plan. Failure to rehab tendinopathy patients results in unhappy patients and possibly chronic pain. While eccentric exercise may elicit pain, if it is not above a four out of ten and does not radiate peripherally, the patient should continue to perform sets and reps as directed.
The benefits are clear:
A British Journal of Sports Medicine study demonstrated that five 45-second isometric quadriceps contractions held at 70% maximum contraction provided almost complete relief of patellar tendon pain immediately and for at least 45 minutes. (9)
5. Surgery As A First Option
Surgery is not an option unless your patient corrects the first four variables without alleviating symptoms. If a patient rushes to surgery before relieving the repetitive stress or educating the patient on the importance of rest and daily rehab, re-rupture is inevitable. Re-injury often occurs because scarring from surgery results in weakened tendon tissue! The exact problem that you and your patient started with. (2)
Stop guessing with your patients on the right rehab or treatment for these patients. If you need some brushing up on all the evidence surrounding the treatment and evaluation of Patellar Tendinopathy, check out the condition reference section in ChiroUp. If you want to provide the best exercises and ADL information to your next patient with Patellar Tendinopathy, download this Condition report to help your patients recover quickly.
And if you aren’t yet a ChiroUp subscriber, get started now for FREE! You, too, can deliver the most up-to-date treatment plans for your patients in as little as 4 clicks!
-
Kaux, J. F., Forthomme, B., Goff, C. L., Crielaard, J. M. & Croisier, J. L. Current opinions on tendinopathy. J. Sports Sci. Med. 10, 238–253 (2011).
Nourissat, G., Berenbaum, F., & Duprez, D. (2015). Tendon injury: from biology to tendon repair. Nature Reviews Rheumatology, 11(4), 223–233. doi:10.1038/nrrheum.2015.26
Ferretti A, Papandrea P, Conteduca F. Knee injuries in volleyball. Sports Medicine. 1990 Aug 1;10(2):132-8
Cushman DM, Petrin Z, Eby S, Clements ND, Haight P, Snitily B, Teramoto M. Ultrasound evaluation of the patellar tendon and Achilles tendon and its association with future pain in distance runners. The Physician and Sportsmedicine. 2021 Oct 2;49(4):410-9.
Earp JE, Gesick H, Angelino D, Adami A. Effects of Isometric Loading Intensity on Patellar Tendon Microvascular Response. Scandinavian Journal of Medicine & Science in Sports.
Steffen D, Mienaltowski MJ, Baar K. Scleraxis and Collagen I Expression Increase Following Pilot Isometric Loading Experiments in a Rodent Model of Patellar Tendinopathy. Matrix Biology. 2022 Mar 28.
Killian, M. L., Cavinatto, L., Galatz, L. M. & Thomopoulos, S. The role of mechanobiology in tendon healing. J. Shoulder Elbow Surg. 21, 228–237 (2012).
Challoumas D, Pedret C, Biddle M, Ng NY, Kirwan P, Cooper B, Nicholas P, Wilson S, Clifford C, Millar NL. Management of patellar tendinopathy: a systematic review and network meta-analysis of randomised studies. BMJ Open Sport & Exercise Medicine. 2021 Nov 1;7(4):e001110. Link
Breda SJ, Oei EH, Zwerver J, Visser E, Waarsing E, Krestin GP, de Vos RJ. Effectiveness of progressive tendon-loading exercise therapy in patients with patellar tendinopathy: a randomised clinical trial. British journal of sports medicine. 2021 May 1;55(9):501-9