Sleep Dysfunction and Chronic Pain: A Missing Link to Recovery
As evidence-based chiropractors, we spend considerable time discussing spinal biomechanics, load management, and motor control. Yet, one silent driver of musculoskeletal dysfunction often goes under-recognized: sleep dysfunction.
Recent research suggests that nearly 40% of adults experience disrupted sleep. (1) Among patients with spinal pain, approximately 53% meet the criteria for clinical sleep dysfunction. (2) If we are not screening for sleep, we may be missing a significant contributor to the very pain and disability we are trying to treat.
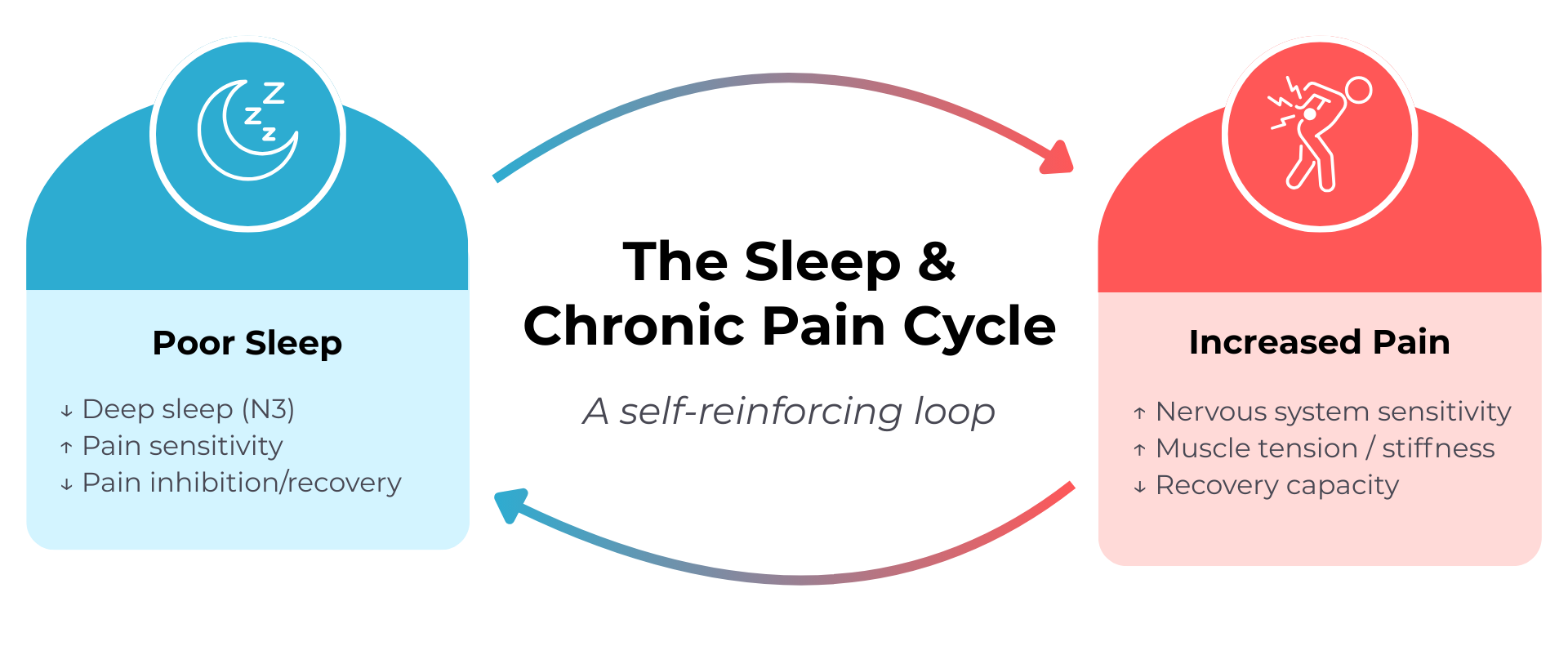
The Bidirectional Relationship Between Sleep and Pain
The relationship between sleep and pain is a bidirectional cycle, not a one-way street.
Sleep → Pain: Sleep deprivation increases pain sensitivity (hyperalgesia) and impairs descending pain inhibitory pathways that are critical for nervous system regulation.
Pain → Sleep: Conversely, persistent MSK pain disrupts sleep quality and duration, making it more challenging to achieve restorative stages such as N3 (deep sleep).
The Predictor: In a study of over 48,000 individuals, sleeplessness was one of the strongest predictors of future chronic pain development—often preceding the onset of pain. (3)
Sleep Screening Framework for Chiropractors
You do not need to be a sleep specialist to improve patient outcomes. A structured approach helps determine when to intervene and when to refer.
1. Screen for the “Big Three” Sleep Disorders
While we do not diagnose sleep disorders, we should screen for these common conditions to guide appropriate referrals:
Insomnia: Difficulty initiating or maintaining sleep greater than 3 nights per week for at least 3 months.
Obstructive Sleep Apnea (OSA): Loud snoring, witnessed gasping, or elevated BMI/neck circumference (screened via STOP-BANG tool).
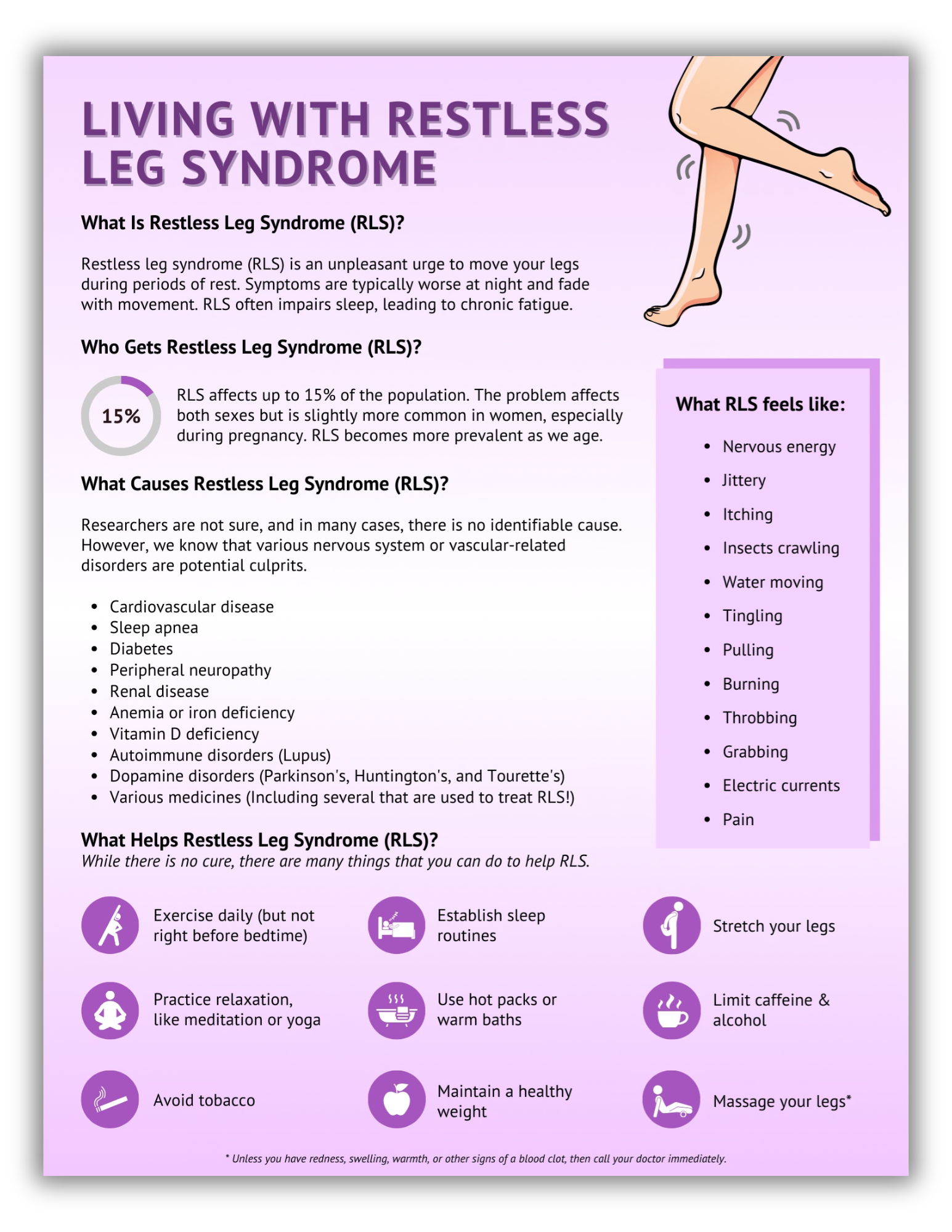
Restless Leg Syndrome (RLS): An uncomfortable urge to move the legs in the evening, relieved by movement.
Related resource: ChiroUp subscribers can download and share the Restless Leg Syndrome infographic in the Forms Library to help educate patients and social media followers.
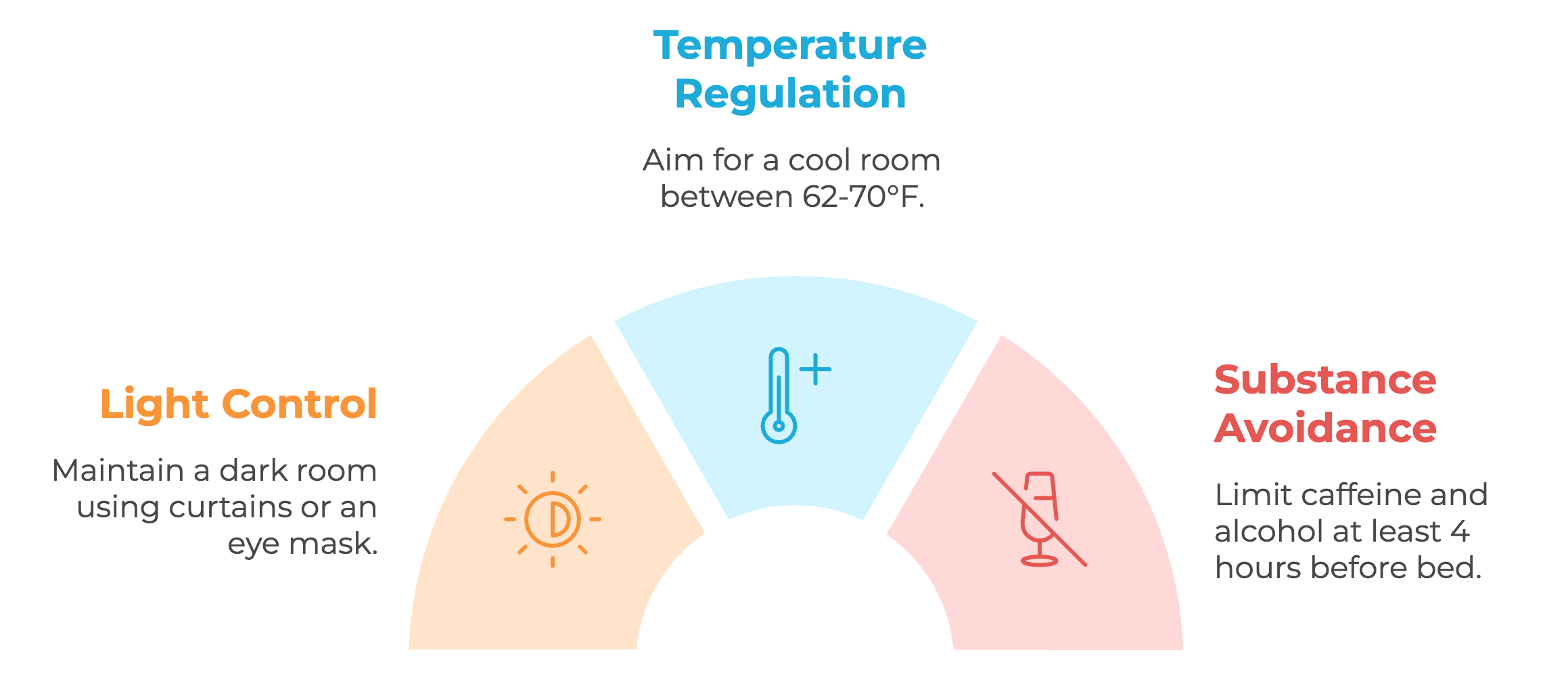
2. Optimize the Sleep Environment
Although “sleep hygiene” has limited effectiveness as a standalone treatment for insomnia (1), it is a valuable adjunct to broader behavioral strategies. (4)
Light: Keep the bedroom dark using blackout blinds or an eye mask; during the sleep period, light at the eye should ideally be less than 1 lux (moonlight).
Temperature: Aim for a cool room, ideally 62–70°F.
Substances: Avoid caffeine at least 4 hours before bed and limit alcohol, as both can disrupt sleep.
Related resource: ChiroUp subscribers can download and share our Healthy Sleep infographic in the Forms Library to help patients build healthier sleep habits that support pain recovery.
3. Behavioral “Quick Wins” Using CBT-I Principles
Incorporating foundational elements of Cognitive Behavioral Therapy for Insomnia (CBT-I) can produce meaningful improvements in both sleep and pain outcomes:
Reduce Pre-Sleep Arousal: While screen light has only a modest effect on sleep onset (≈10-minute delay), stimulating content and “sleep procrastination” are the real disruptors. Encourage a structured "wind-down" period.
Entrain Circadian Rhythms: Maintaining a consistent wake time (within ~1 hour, even on weekends) is one of the most powerful anchors for the internal clock.
Increase Sleep Drive: Promote daytime activity and discourage long naps (limit to 20–30 minutes) to build adequate "sleep pressure".
Note: Avoid vigorous exercise within ~1 hour of bedtime.
The Bottom Line
Poor sleep is not merely a consequence of pain; it is a parallel driver of pain and disability. By routinely screening for sleep health and integrating basic behavioral strategies, evidence-based chiropractors can provide a more comprehensive, patient-centered approach to chronic pain management.
If you’re looking to make sleep screening and patient education easier to implement, ChiroUp can help. Our evidence-based tools are built to support comprehensive, patient-centered care without adding friction to your workflow.
Click the button below to get FREE access to ChiroUp.
Want more? Our top-rated chiropractic podcast covers a wide range of practical clinical topics, including our recent deep dive into sleep and its role in patient recovery. If you haven’t checked it out yet, do it now and be sure to subscribe so you don’t miss future insights that can elevate your practice! Icon and link
-
Shepherd MH, Neilson BD, Siengsukon CF. The Pain of Poor Sleep: A Clinician’s Guide to Assessing and Addressing Sleep Dysfunction in People With Musculoskeletal Pain Conditions. JOSPT Open. 2026 Jan;4(1):1-27.
Neilson BD, Shepherd MH, Dickerson C, Chaconas EJ, Young JL, Rhon DI. Relationship between attitudes and beliefs about sleep, sleep disturbance, and pain interference in patients with spinal pain. The Clinical Journal of Pain. 2022 Aug 1;38(8):541-9.
Fillingim, M., Tanguay-Sabourin, C., Parisien, M. et al. Biological markers and psychosocial factors predict chronic pain conditions. Nat Hum Behav9, 1710–1725 (2025).
Potter GD, Grosicki GJ, Tinsley GM, Wood TR, Garner D, Galpin AJ. Dreamy Dwellings: How the Sleep Environment Affects Sleep Health in Adults—A Narrative Review. Lifestyle Medicine. 2025 Oct;6(4):e70022.