Schmorl’s Node Refresher: 7 Surprising Facts Every DC Must Own
Are you interested in the latest buzz surrounding Schmorl's nodes? Want to gain new insights in less than five minutes? You're in the right place! Welcome to our ultimate Schmorl's Nodes refresher that keeps you in the know. Let’s pop right in. 😏
1. What is a schmorl’s node?
A Schmorl’s node (aka intraosseous disc herniation or intravertebral disc herniation) represents an area where the disc nucleus has herniated through the cartilaginous vertebral endplate. (1) The lesion appears on imaging as a well-defined, small, round or oval radiolucent vertebral indentation, often with a thin rim of sclerosis. (2)
Schmorl node facts:
Most common sites include the T7-L1 region, although any region is vulnerable, including the cervical spine. (3,4)
Average size is 7 × 9 mm, but this varies from minimally noticeable protrusions to large prominent indentations (5)
Approximately two-thirds affect the inferior endplate (3)
Typically impact the central or posterior portion of the endplate (1,3)
Schmorl’s nodes are best visualized on MRI or CT, but approximately 33% can also be seen on plain X-rays. (2,7)
Schmorls node spine MRI
Schmorl’s node lumbar spine x-ray
2. How common are schmorl’s nodes?
The reported frequency of schmorl’s nodes varies from 2–80%. (8-17) This uselessly extensive range is likely attributed to how the prevalence was measured in each study, i.e., calculating prevalence on plain films will yield lower estimates than measuring on advanced imaging or post-mortem assessments.
Experienced clinicians will confirm that schmorl’s nodes are relatively frequent benign findings.
3. What are the causes of schmorl’s nodes?
Spinal load + vertebral endplate vulnerability
Traumatic vertebral axial loading is a primary culprit. (1,18,19) One study concluded that 93% of acute, symptomatic endplate smorl’s node presentations included an identifiable traumatic onset, i.e., vehicular or sports injury, fall, etc. (20) The incidence of schmorl’s nodes is nearly twice as high in elite gymnasts as compared to non-athletes. (19) Not surprisingly, since axial load increases as we descend along the spine, the lower spine is most commonly affected.
Factors that weaken the vertebral architecture can increase the likelihood of developing a schmorl’s node. Although these factors are thought to be contributory to only a small percentage of cases, potential culprits include osteopenia, smoking (OR-3.2), congenital ossification gaps, Padget’s disease, autoimmune disease, ischemic necrosis, metabolic disease, malignancy, infection, inflammation (Modic changes), hyperparathyroidism, and Scheuermann’s disease. (6,8,13,21-25)
Any discussion of Schmorl’s node causes should also mention disc hydration status since a well-hydrated nucleus has more volume to punch an endplate defect when loaded. Thus, young patients with well-hydrated discs may be most vulnerable. This theory is further supported by several studies showing that the incidence of schmorl’s nodes does not increase appreciably with age. (16,26,27)
4. How can a disc nucleus cause an endplate fracture?
Schmorl’s node formation occurs via nuclear herniation through an endplate. To fully understand this process, you’ll first want to see what a disc nucleus looks like.
What is the consistency of the disc nucleus? Watch this one-minute video.
Your next logical question is, how can fluid fracture a bone? Two studies provide significant clues:
“The nucleus pulposus exhibited significant viscoelastic effects, characteristic of a fluid and a solid. Whether the nucleus pulposus behaves more as a fluid or a solid in vivo depends on the rate of loading.” (28)
“A log-linear relationship between intervertebral disc stiffness and strain rate was observed.” (29)
This means the disc nucleus becomes stiffer as the load rate increases. Watch this 60-second live demo of how a jelly-like nucleus instantly changes to a consistency that can dent bone.
5. What are the symptoms of schmorl’s nodes?
Do schmorls nodes cause pain?
Historically, schmorl’s nodes have been considered asymptomatic, incidental findings. (38) However, significant research has found a symptomatic relationship, including pain and limited function. (25,26,39)
“The presence of endplate defects was associated with 1.64 times increased risk of lifetime back pain.” (8)
Back pain patients are three times more likely to exhibit schmorls nodes than asymptomatic groups. (30)
“The presence of Schmorl's nodes was associated with neck pain." (31)
While chronic schmorls nodes that lack adjacent vertebral edema may be asymptomatic (18,32), acute presentations with accompanying inflammation would likely trigger a “symptom sandwich”:
Stage 1 - Avascular “foreign” nuclear material abruptly injected into a highly vascular vertebral body is not typically appreciated by the immune system. An acutely inflamed endplate fracture triggers non-radicular back pain and tenderness. (18,20) Acute defects sometimes start following an abrupt axial load (i.e., jumping off an elevated surface) followed by a painful “pop.” Acute schmorls node pain is provoked by trunk movement and may occasionally refer to the abdomen or thighs. (20) Acute schmorl's node symptoms in chronic LBP patients may present as an exacerbation that is “different.”
Stage 2 - Symptoms subside as fatty marrow changes and sclerosis replace acute inflammation. This process typically spans 3-18 months. (1,20)
Stage 3 - Annular degeneration follows schmorls node development. (33) Degenerative changes of the overloaded annulus and facets accelerate after support from the central nuclear material is absent. One study found that Schmorl’s node patients had “approximately 7-fold increased risk of severe intervertebral disc degeneration at the corresponding levels." (30)
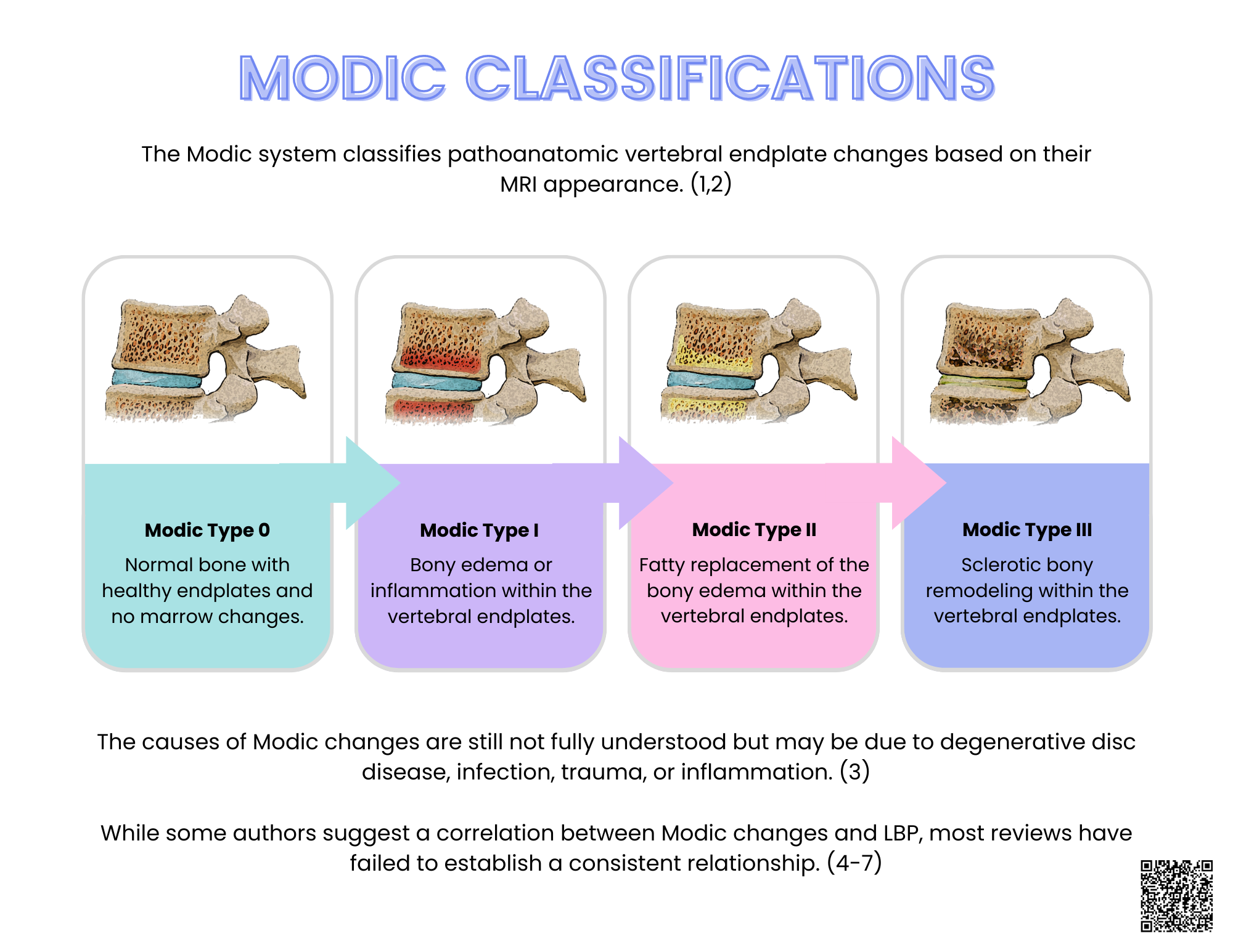
This process mirrors Modic changes, which is unsurprising since endplate microfractures can trigger Modic changes. (34,35) To learn more, check out this past blog and infographic on Demystifying Modic Changes.
6. How to treat schmorl’s nodes
Schmorl’s node treatment is typically conservative. (2,9,26)
“In both asymptomatic and symptomatic patients, the mainstay of treatment for Schmorl’s nodes is conservative therapy.” (6)
Clinicians might manage acute schmorls nodes similar to a compression fracture. (36) Considerations include anti-inflammatory measures, bracing, soft-tissue therapy, nutritional support (particularly vitamin D and calcium in older patients), and progressive aerobic and therapeutic exercise as tolerated. (37) Patients sometimes need to be reminded that an acute schmorl’s node represents a fracture, and a period of relative rest may be necessary. (20)
Chronic schmorls nodes are often considered incidental findings. Management would address concurrent biomechanical issues and mitigate the impending degenerative changes.
7. How do I educate my patients about Schmorl’s nodes?
We made this one simple. Use the new ChiroUp lay infographic to answer your patient’s foremost questions quickly.
What is a schmorl’s node?
Is a schmorl’s node serious?
Do schmorls nodes cause pain?
What can be done for schmorl’s node?
As a subscriber you’ll be able to find this infographic in the forms library by searching “Schmorl’s”. Not a ChiroUp subscriber? Set up your FREE account today!
-
1. Abu-Ghanem S, Ohana N, Abu-Ghanem Y, Kittani M, Shelef I. Acute schmorl node in dorsal spine: an unusual cause of a sudden onset of severe back pain in a young female. Asian spine journal. 2013 Jun;7(2):131. Link
2. Pietrok A, Lee C, Kaye RJ, Kaye AD, Chesteen G. Schmorl’s Node: An Uncommon Case of Back Pain and Radiculopathy. Orthopedic Reviews. 2022;14(3). Link
3. Hamanishi C, Kawabata T, Yosii T, Tanaka S. Schmorl's nodes on magnetic resonance imaging: their incidence and clinical relevance. Spine. 1994 Feb 1;19(4):450-3. Link
4. Jagannathan D, Indiran V, Hithaya F. Prevalence and clinical relevance of Schmorl’s nodes on magnetic resonance imaging in a tertiary hospital in Southern India. Journal of clinical and diagnostic research: JCDR. 2016 May;10(5):TC06. Link
5. Wu HT, Morrison WB, Schweitzer ME. Edematous Schmorl’s nodes on thoracolumbar MR imaging: characteristic patterns and changes over time. Skeletal radiology. 2006 Apr;35:212-9. Link
6. Pietrok A, Lee C, Kaye RJ, Kaye AD, Chesteen G. Schmorl’s Node: An Uncommon Case of Back Pain and Radiculopathy. Orthopedic Reviews. 2022;14(3). Link
7. Hamanishi C, Kawabata T, Yosii T, Tanaka S. Schmorl's nodes on magnetic resonance imaging: their incidence and clinical relevance. Spine. 1994 Feb 1;19(4):450-3. Link
8. Chen L, Battié MC, Yuan Y, Yang G, Chen Z, Wang Y. Lumbar vertebral endplate defects on Magnetic Resonance Images: Prevalence, distribution patterns, and associations with back pain. The Spine Journal. 2019 Oct 25. Link
9. Diehn FE, Maus TP, Morris JM, Carr CM, Kotsenas AL, Luetmer PH, Lehman VT, Thielen KR, Nassr A, Wald JT. Uncommon manifestations of intervertebral disk pathologic conditions. Radiographics. 2016 May;36(3):801-23. Link
10. Hamanishi C, Kawabata T, Yosii T, Tanaka S. Schmorl's nodes on magnetic resonance imaging: their incidence and clinical relevance. Spine. 1994 Feb 1;19(4):450-3. Link
11. Stäbler A, Bellan M, Weiss M, Gärtner C, Brossmann J, Reiser MF. MR imaging of enhancing intraosseous disk herniation (Schmorl's nodes). AJR. American journal of roentgenology. 1997 Apr;168(4):933-8. Link
12. Hilton RC, Ball J, Benn RT. Vertebral end-plate lesions (Schmorl's nodes) in the dorsolumbar spine. Annals of the rheumatic diseases. 1976 Apr 1;35(2):127-32. Link
13. Schmorl G. The human spine in health and disease. InThe human spine in health and disease 1971 (pp. xi-504). Link
14. Frymoyer JW, Newberg A, Pope MH, Wilder DG, Clements J, MacPherson B. Spine radiographs in patients with low-back pain. An epidemiological study in men. JBJS. 1984 Sep 1;66(7):1048-55. Link
15. Dar G, Masharawi Y, Peleg S, Steinberg N, May H, Medlej B, Peled N, Hershkovitz I. Schmorl’s nodes distribution in the human spine and its possible etiology. European Spine Journal. 2010 Apr;19:670-5. Link
16. Sonne-Holm S, Jacobsen S, Rovsing H, Monrad H. The epidemiology of Schmorl’s nodes and their correlation to radiographic degeneration in 4,151 subjects. European spine journal. 2013 Aug;22:1907-12. Link
17. Burke KL. Schmorl’s nodes in an American military population: Frequency, Formation, and Etiology. Journal of forensic sciences. 2012 May;57(3):571-7. Link
18. Wagner AL, Murtagh FR, Arrington JA, Stallworth D. Relationship of Schmorl's nodes to vertebral body endplate fractures and acute endplate disk extrusions. American Journal of Neuroradiology. 2000 Feb 1;21(2):276-81. Link
19. Swärd LE, Hellström MI, Jacobsson BO, Nyman RI, Peterson LA. Disc degeneration and associated abnormalities of the spine in elite gymnasts: a magnetic resonance imaging study. Spine. 1991 Apr 1;16(4):437-43. Link
20. Paterakis KN, Brotis AG, Dardiotis E, Hadjigeorgiou GM, Karachalios T, Fountas KN, Karantanas A. Acute Schmorl's node during strenuous monofin swimming: a case report and review of the literature. Global spine journal. 2012 Sep;2(3):159-67. Link
21. Sonne-Holm S, Jacobsen S, Rovsing H, Monrad H. The epidemiology of Schmorl’s nodes and their correlation to radiographic degeneration in 4,151 subjects. European spine journal. 2013 Aug;22:1907-12. Link
22. Mok FP, Samartzis D, Karppinen J, Luk KD, Fong DY, Cheung KM. ISSLS prize winner: prevalence, determinants, and association of Schmorl nodes of the lumbar spine with disc degeneration: a population-based study of 2449 individuals. Spine. 2010 Oct 1;35(21):1944-52. Link
23. Jang JS, Kwon HK, Lee JJ, Hwang SM, Lim SY. Rami communicans nerve block for the treatment of symptomatic Schmorl's nodes-a case report. The Korean journal of pain. 2010 Dec 1;23(4):262-5. Link
24. Peng B, Wu W, Hou S, Shang W. The pathogenesis of Schmorl’s nodes. The Journal of Bone & Joint Surgery British Volume. 2003 Aug 1;85(6):879-82. Link
25. Hershkovich OD, Koch JE, Grevitt MP. Schmorl node—a cause of acute thoracic pain: a case report and pathophysiological mechanism. International Journal of Spine Surgery. 2020 Jun 1;14(3):441-6. Link
26. Kyere KA, Than KD, Wang AC, Rahman SU, Valdivia–Valdivia JM, La Marca F, Park P. Schmorl’s nodes. European Spine Journal. 2012 Nov;21:2115-21. Link
27. Hilton RC, Ball J, Benn RT. Vertebral end-plate lesions (Schmorl's nodes) in the dorsolumbar spine. Annals of the rheumatic diseases. 1976 Apr 1;35(2):127-32. Link
28. Iatridis JC, Weidenbaum M, Setton LA, Mow VC. Is the nucleus pulposus a solid or a fluid? Mechanical behaviors of the nucleus pulposus of the human intervertebral disc. Spine. 1996 May 15;21(10):1174-84. Link
29. Newell N, Carpanen D, Grigoriadis G, Little JP, Masouros SD. Material properties of human lumbar intervertebral discs across strain rates. The Spine Journal. 2019 Dec 1;19(12):2013-24. Link
30. Ekşi MŞ, Turgut VU, Berikol G, Özmen BB, Huet SE, Dinç T, Küçüksüleymanoğlu D, Orhun Ö, Özcan-Ekşi EE. Schmorl’s nodes could be associated with intervertebral disc degeneration at upper lumbar levels and end-plate disease at lower lumbar level in patients with low back pain. Journal of Clinical Neuroscience. 2022 Jun 1;100:66-74. Link
31. Otaki H, Otani K, Watanabe T, Sekiguchi M, Konno SI. Associations between clinical neck symptoms and various evaluations ofcervical intervertebral disc degeneration by magnetic resonance imaging. Fukushima journal of medical science. 2021. Link
32. Borne J, Daniels DL. Guidelines for differentiating vertebral marrow abnormalities on MRI. MRI decisions. 1991;5(6):2-18. Link
33. Ogon I, Takashima H, Morita T, Oshigiri T, Terashima Y, Yoshimoto M, Fukushi R, Fujimoto S, Emori M, Teramoto A, Takebayashi T. Relevance between Schmorl’s node and lumbar intervertebral disc degeneration quantified with magnetic resonance imaging T2 mapping in chronic low back pain. Asian Spine Journal. 2020 Oct;14(5):621. Link
34. Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988 Jan;166(1):193-9. Link
35. Gaillard F, Hapugoda S, Murphy A, et al. Modic type I endplate change. Reference article, Radiopaedia.org (Accessed on 14 Jun 2023) from Link
36. Jang JS, Kwon HK, Lee JJ, Hwang SM, Lim SY. Rami communicans nerve block for the treatment of symptomatic Schmorl's nodes-a case report. The Korean journal of pain. 2010 Dec 1;23(4):262-5. Link
37. ChiroUp.com. Osteoporotic Vertebral Compression Protocol. Link
38. Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. New England Journal of Medicine. 1994 Jul 14;331(2):69-73. Link
39. Williams FM, Manek NJ, Sambrook PN, Spector TD, MacGregor AJ. Schmorl's nodes: common, highly heritable, and related to lumbar disc disease. Arthritis Care & Research: Official Journal of the American College of Rheumatology. 2007 Jun 15;57(5):855-60. Link