Managing Patellofemoral Pain Syndrome: New Research Insights and Treatment Strategies
Patellofemoral pain affects nearly one-fourth of the population each year, with females experiencing almost double the risk of males. (1,2) The condition accounts for approximately 7% of all medical diagnoses. (3)
Fortunately, evidence-based chiropractors are well-equipped to manage patellofemoral pain syndrome (PFPS). This blog will highlight the most essential clinical pearls from the past year of research, including a dozen systematic reviews. In less than 5 minutes, you’ll learn valuable new clinical skills for managing this common presentation.
1. What are the symptoms of patellofemoral pain syndrome?
The cardinal symptom of patellofemoral pain syndrome, aka “Runner’s Knee,” is anterior knee pain that intensifies with weight-bearing activity, particularly during activities that load the joint, including prolonged walking, running, squatting, jumping, kneeling, arising from a seated position or stair climbing- especially walking down stairs or downhill. (4,5)
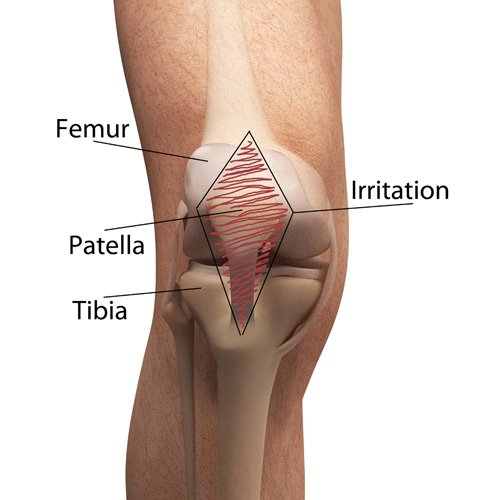
2. What causes patellofemoral pain syndrome?
Patellofemoral pain typically develops from a combination of cartilage vulnerability, improper biomechanics, and demanding activity, i.e., squats, stair climbing, running, etc. *If you’re a numbers nerd and are looking for a deeper dive, The American Journal of Sports Medicine (6) recently quantified activity and exercise-related patellofemoral load.
The patella naturally tends to migrate laterally due to the pull of the quadriceps and the slight natural valgus of the lower extremity. (7) This causes a “lateral patellar tracking disorder” where the lateral patellar facet rubs against the lateral femoral condyle. This compression is often compounded by one or more of the following biomechanical functional deficits.
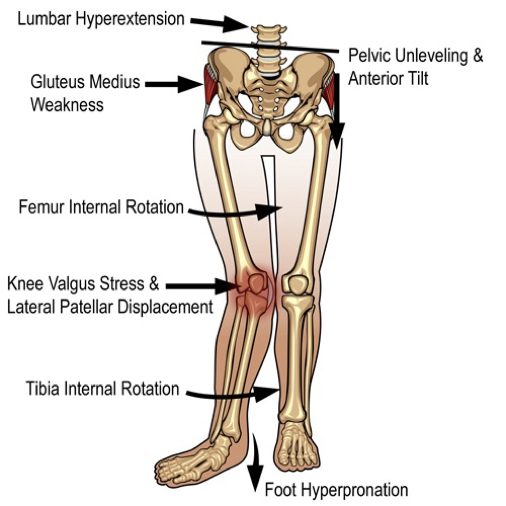
Gluteus medius weakness
Patellofemoral pain syndrome patients consistently demonstrate hip abductor weakness with resultant kinematic problems, particularly uncontrolled hip adduction when ambulating. (8-13) Biomechanical studies have shown that excessive hip adduction is the “[primary] biomechanical variable associated with running injury.” (14) Some debate persists as to whether hip abductor weakness is a cause or a symptom of patellofemoral pain syndrome; however, this argument is largely inconsequential since rehabbing hip abductor weakness is essential, regardless. (15)
ITB tightness
Multiple studies have found that patellofemoral pain syndrome patients’ ITB and lateral retinaculum are tighter and thicker. (16-19) Excessive tightness in the ITB and lateral retinaculum are thought to contribute to patellar mal-tracking by limiting medial centration. (15)
Foot hyperpronation
Loss of the longitudinal arch causes internal rotation of the tibia and subsequent deviation of the patella, increasing one's risk of patellofemoral pain syndrome. (20-26)
Gait deficits
Runners with slow cadence or excessively narrow gait patterns (i.e., crossover gait) are predisposed to patellofemoral pain syndrome. Additionally, running with a rear-foot strike imposes higher loads on the knee and patellofemoral joints. In contrast, a forefoot strike transitions the load toward the ankle joint and Achilles tendon. (27)
Wildcard ⚠️: VMO weakness
VMO atrophy is inconsistently present in patellofemoral pain syndrome patients, although a causal relationship has not been established. (15,28-30)
3. How do you evaluate patellofemoral pain syndrome?
Watch this patellofemoral pain syndrome assessment tutorial for the top patellofemoral pain syndrome tests.
PFPS is primarily a diagnosis of exclusion, and the following tests can help solidify the diagnosis.
Squatting
The most sensitive physical examination test for patellofemoral pain syndrome patients is pain with squatting. (31) Differentiating meniscal pain from patellofemoral pain may be accomplished by having the patient perform a two-legged squat. Meniscal pain is expected at the bottom of the squat, while patellofemoral pain is present during descent and ascent.
Step test
The step test is performed by placing one foot on a 6-inch block with hands on hips. Using the affected limb, lower your body in a controlled and gradual manner until the heel of the opposite leg touches the floor. This test for patellofemoral pain syndrome reproduces pain in three-fourths (74%) of PFPS patients. (32)
Patellar grind
This PFPS test begins by applying a compressive downward force to the supine patient’s patellofemoral joint. The patient is then asked to contract their quadriceps muscle while the patellofemoral joint is compressed. Pain or crepitus indicates patellofemoral irritation. Patients with a positive grind test are significantly more likely to develop subsequent knee osteoarthritis. (34) *Clinicians should use caution when performing this test, not unnecessarily to provoke pain or create new irritation.
Patellar mobility
Patellar mobility may be assessed with the Patellar Glide test and Patellar tilt test or by observing patellar tracking during active knee flexion/extension. (35)
ChiroUp subscribers can review any of the tests mentioned above in their Clinical Skills tab.
If you’re not yet a subscriber to the ChiroUp platform and would like to learn more, book a 20-minute discovery call with a member of our team.
Functional assessment
Examining a patient's gait, posture, and footwear can help identify patellofemoral pain syndrome triggers. (36) Clinicians should be particularly observant of foot hyperpronation, which primarily contributes to patellar mal-tracking. Gluteus medius (hip abductor) weakness may be assessed by observing for pelvic drop or knee valgus (Trendelenberg sign) when performing a single-leg stand, single-leg squat, or single-leg 6” step down.
Deeper dive: Check out these on-demand ChiroUp webinars for common functional deficits:
Wildcard ⚠️: Radiographs
Plain radiographs of the knee are generally unnecessary for the simple diagnosis of patellofemoral pain syndrome but can exclude other more advanced diagnoses, such as osteoarthritis, patellar fracture, and osteochondritis. (31)
4. What are the top patellofemoral pain syndrome treatments?
Here are nine evidence-based, in-office treatments for patellofemoral pain syndrome.
Exercise
Per the 2016 consensus statement by the International Patellofemoral Pain Research Committee, exercise therapy is considered the primary treatment approach for individuals with PFPS (37). Due to the multifactoral etiology of patellofemoral pain syndrome, a combination of hip and knee exercises is most beneficial. (36,38)
Whole-Body Vibration
Combining whole-body vibration with exercise may lead to more significant pain reduction than exercise alone in patellofemoral pain syndrome patients. (39)
BFR
While the evidence on Blood Flow Restriction exercise is inconclusive, some researchers have found that BFR improves pain and function for patients with patellofemoral pain syndrome. (15,40) Additionally, combining BFR and IASTM has been shown to be more effective than either therapy in isolation. (41)
What is BFR?
BFR, or blood flow restriction training, is a technique that involves partially restricting blood flow to a muscle group while performing exercises at a lower intensity than traditional strength training. This restriction is typically achieved using a tourniquet or adjustable bands applied to the limb with about 70% pressure. By limiting blood flow, BFR creates a hypoxic environment in the muscles, which triggers a cascade of physiological adaptations that lead to increased strength, muscle growth, and improved endurance. (15)
Manipulation
Manipulation of the lumbar spine, hip, sacroiliac joint, knee, and ankle regions may benefit patellofemoral pain syndrome patients. (43,44) Mobilization and manipulation of the patellofemoral and tibiofemoral joints may provide benefits for PFPS patients. (5,36,45) Research has shown that lumbopelvic manipulation can improve knee pain, knee position sense, and balance in patients with patellofemoral pain. (46)
Myofascial release
Myofascial release and stretching should be directed at hypertonic muscles, including the TFL, gastrocnemius, soleus, hamstring, piriformis, hip rotators, and psoas.
IASTM
IASTM may be appropriate for tightness in the iliotibial band, vastus lateralis, posterior hip capsule, and lateral knee retinaculum. Research indicates that IASTM treatment can enhance knee pain relief, improve muscle flexibility, and increase knee strength without pain. (41)
Dry needling
Research has shown that dry needling plus stretching outperforms prescription NSAIDs and stretching, providing superior and longer-lasting effects lasting at least six months. (47)
Therapeutic Taping
There is conflicting evidence concerning the effectiveness of traditional patellofemoral taping, i.e., McConnel taping. (48-52) Studies on elastic therapeutic tape are also mixed but encouraging. (79-81) Taping, including exercise, is most useful in a comprehensive, multi-modal treatment approach. (36)
Orthotics
Foot orthotics may be beneficial in reducing pain and improving function in patellofemoral pain syndrome patients. (36, 53-55,78).
Wildcard ⚠️: EMS
A 2017 Cochrane Review found limited, low-quality evidence regarding the effectiveness of e-stim for patellofemoral pain syndrome treatment, suggesting a slight reduction in pain but insufficient support for improvements in strength or function. (56).
5. What are the best exercises for patellofemoral pain syndrome?
Since hip abductor weakness is a critical factor in developing patellofemoral pain syndrome, strengthening exercises targeting the gluteus medius prove most effective, leading to decreased pain and improved function. (54,57-65) Potential exercises would include:
Patellofemoral pain syndrome rehab should include progressive hip and knee strengthening with open and closed-chain exercises. (6,36) In addition to correcting underlying functional triggers, a straightforward, progressive program might consider the following progression (6):
Walking
Seated knee extension
Low step up
Low step-down
60° double-leg squat
High step-up
Single-leg squat
Sports-related activity
6. What are the essential ADLs for patellofemoral pain syndrome?
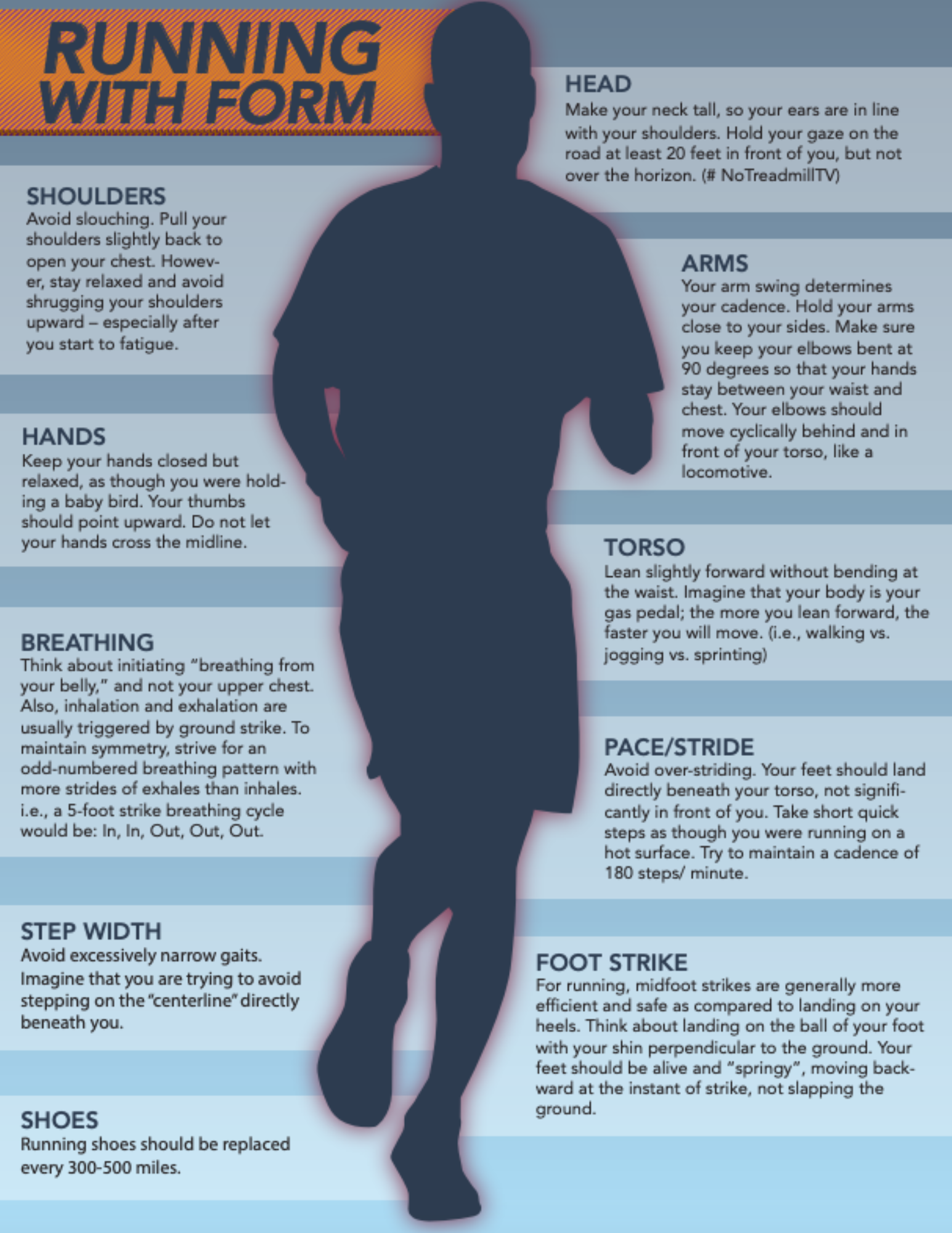
Gait Training
Training patellofemoral pain syndrome patients to increase their step rate by 10% produces lasting improvements in pain and function. (66-69) Selecting moderate running speeds (~3.1 m/s) with reduced training duration or an interval-based approach may be more effective for managing cumulative patellofemoral joint kinetics than running at slow speeds. (70)
Footwear
Runners should change shoes every 250 to 500 miles. Running shoes with less than 5mm heel drop decreased patellofemoral joint stress significantly by reducing total knee extension. (71) Running shoes with less than 5mm heel drop decrease patellofemoral joint stress significantly by reducing total knee extension. (72) Providers should counsel runners on choosing between motion-control, cushioned, stability, or neutral shoes. See this prior Running blog for details.
10% rule
One study found that those who abruptly increased their training mileage by more than 30% over two weeks were more susceptible to injury (73). In particular, new runners are vulnerable to breaking the “10% rule”, i.e., do not increase any activity by more than 10% from the previous level. (15)
PNE
Recent studies suggest that patellofemoral pain syndrome is not solely a peripheral issue but also involves central sensitization, as evidenced by heightened pain perception and hyperalgesia in affected individuals (74-76). This highlights the need for a multi-faceted approach that addresses both physical and psychological factors, as corroborated by a systematic review linking patellofemoral pain syndrome to increased anxiety, depression, catastrophizing, and fear of movement (77).
Wouldn’t having a professional content and graphic design team that could create potent infographics to educate your patients be great? Well, ChiroUp’s got you covered.
ChiroUp will help you enhance the way you communicate and educate your patients. This will lead to stronger compliance, better outcomes, and higher satisfaction.
ChiroUp subscribers can download the following infographics from their forms library by searching the name of the infographic.
-
1. Smith BE, Selfe J, Thacker D, Hendrick P, Bateman M, Moffatt F, Rathleff MS, Smith TO, Logan . Incidence and prevalence of patellofemoral pain: a systematic review and meta-analysis. PloS one. 2018 Jan 11;13(1):e0190892. Link
2. Glaviano NR, Mangum LC, Bazett-Jones DM, DiStefano LJ, Toland MD, Boling M. Strength Training Rehabilitation Incorporating Power Exercises (STRIPE) for individuals with patellofemoral pain: a randomised controlled trial protocol. BMJ open sport & exercise medicine. 2023 Jan 1;9(1):e001482. Link
3. Glaviano NR, Kew M, Hart JM, Saliba S. Demographic and epidemiological trends in patellofemoral pain. International journal of sports physical therapy. 2015 Jun;10(3):281. Link
4. Thomeé R, Augustsson J, Karlsson J. Patellofemoral pain syndrome. Sports medicine. 1999 Oct 1;28(4):245-62. Link
5. Lantz JM, Emerson-Kavchak AJ, Mischke JJ, Courtney CA. Tibiofemoral joint mobilization in the successful management of patellofemoral pain syndrome: a case report. International journal of sports physical therapy. 2016 Jun;11(3):450. Link
6. Song K, Scattone Silva R, Hullfish TJ, Silbernagel KG, Baxter JR. Patellofemoral Joint Loading Progression Across 35 Weightbearing Rehabilitation Exercises and Activities of Daily Living. The American Journal of Sports Medicine. 2023:03635465231175160. Link
7. Wilson T. The measurement of patellar alignment in patellofemoral pain syndrome: are we confusing assumptions with evidence?. journal of orthopaedic & sports physical therapy. 2007 Jun;37(6):330-41. Link
8. Xie P, István B, Liang M. The Relationship between Patellofemoral Pain Syndrome and Hip Biomechanics: A Systematic Review with Meta-Analysis. InHealthcare 2022 Dec 28 (Vol. 11, No. 1, p. 99). MDPI. Link
9. Van Cant J, Pineux C, Pitance L, Feipel V. Hip muscle strength and endurance in females with patellofemoral pain: a systematic review with meta‐analysis. International journal of sports physical therapy. 2014 Oct;9(5):564. Link
10. Prins MR, Van der Wurff P. Females with patellofemoral pain syndrome have weak hip muscles: a systematic review. Australian journal of physiotherapy. 2009 Jan 1;55(1):9-15. Link
11. Nakagawa TH, Moriya ÉT, Maciel CD, SerrãO FV. Trunk, pelvis, hip, and knee kinematics, hip strength, and gluteal muscle activation during a single-leg squat in males and females with and without patellofemoral pain syndrome. Journal of orthopaedic & sports physical therapy. 2012 Jun;42(6):491-501. Link
12. Souza RB, Powers CM. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. Journal of orthopaedic & sports physical therapy. 2009 Jan;39(1):12-9. Link
13. Neal BS, Barton CJ, Birn-Jeffery A, Morrissey D. Increased hip adduction during running is associated with patellofemoral pain and differs between males and females: A case-control study. Journal of Biomechanics. 2019 Jun 25;91:133-9. Link
14. Lopes AD, Mascarinas A, Hespanhol L. Are alterations in running biomechanics associated with running injuries? A systematic review with meta-analysis. Brazilian Journal of Physical Therapy. 2023 Aug 23:100538. Link
15. Sisk D, Fredericson M. Update of risk factors, diagnosis, and management of patellofemoral pain. Current reviews in musculoskeletal medicine. 2019 Dec;12:534-41. Link
16. Schoots EJ, Tak IJ, Veenstra BJ, Krebbers YM, Bax JG. Ultrasound characteristics of the lateral retinaculum in 10 patients with patellofemoral pain syndrome compared to healthy controls. Journal of Bodywork and Movement Therapies. 2013 Oct 1;17(4):523-9. Link
17. Kang SY, Choung SD, Park JH, Jeon HS, Kwon OY. The relationship between length of the iliotibial band and patellar position in Asians. The Knee. 2014 Dec 1;21(6):1135-8. Link
18. Merican AM, Amis AA. Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. Journal of biomechanics. 2009 Jul 22;42(10):1539-46. Link
19. Lack S, Anthony L, Noake J, Brennan K, Zhang B, Morrissey D. Medial and Lateral Patellofemoral Joint Retinaculum Thickness in People With Patellofemoral Pain: A Case‐Control
Study. Journal of Ultrasound in Medicine. 2019 Jun;38(6):1483-90. Link
20. Hetsroni I, Finestone A, Milgrom C, Sira DB, Nyska M, Radeva-Petrova D, Ayalon M. A prospective biomechanical study of the association between foot pronation and the incidence of anterior knee pain among military recruits. The Journal of Bone & Joint Surgery British Volume. 2006 Jul 1;88(7):905-8. Link
21. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. The American journal of sports medicine. 2009 Nov;37(11):2108-16. Link
22. Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, Garrick JG, Hewett TE, Huston L, Ireland ML, Johnson RJ. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2000 May 1;8(3):141-50. Link
23. Bobbert MF, Van Zandwijk JP. Dynamics of force and muscle stimulation in human vertical jumping. Link
24. Zappala FG, Taffel CB, Scuderi GR. Rehabilitation of patellofemoral joint disorders. The Orthopedic Clinics of North America. 1992 Oct;23(4):555-66. Link
25. Boling MC, Padua DA, Marshall SW, Guskiewicz K, Pyne S, Beutler A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: the Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. The American journal of sports medicine. 2009 Nov;37(11):2108-16. Link
26. Petersen W, Rembitzki I, Liebau C. Patellofemoral pain in athletes. Open access journal of sports medicine. 2017;8:143. Link
27. Xu Y, Yuan P, Wang R, Wang D, Liu J, Zhou H. Effects of Foot Strike Techniques on Running Biomechanics: A Systematic Review and Meta-analysis. Sports Health. 2020 Aug 19:1941738120934715. Link
28. Pattyn E, Verdonk P, Steyaert A, Vanden Bossche L, Van den Broecke W, Thijs Y, Witvrouw E. Vastus medialis obliquus atrophy: does it exist in patellofemoral pain syndrome?. The American journal of sports medicine. 2011 Jul;39(7):1450-5. Link
29. Giles LS, Webster KE, McClelland JA, Cook J. Atrophy of the quadriceps is not isolated to the vastus medialis oblique in individuals with patellofemoral pain. journal of orthopaedic & sports physical therapy. 2015 Aug;45(8):613-9. Link
30. Briani RV, de Oliveira Silva D, Pazzinatto MF, Ferreira AS, Ferrari D, de Azevedo FM. Delayed onset of electromyographic activity of the vastus medialis relative to the vastus lateralis may be related to physical activity levels in females with patellofemoral pain. Journal of Electromyography and Kinesiology. 2016 Feb 1;26:137-42. Link
31. Gaitonde DY, Ericksen A, Robbins RC. Patellofemoral Pain Syndrome. Am Fam Physician. 2019 Jan 15;99(2):88-94. Link
32. NNijs J, Van Geel C, Van de Velde B. Diagnostic value of five clinical tests in patellofemoral pain syndrome. Manual therapy. 2006 Feb 1;11(1):69-77. Link
33. Intentionally blank
34. Deng H, Wu Y, Fan Z, Tang W, Tao J. The association between patellofemoral grind and synovitis in knee osteoarthritis: data from the osteoarthritis initiative. Frontiers in Medicine. 2023;10. Link
35. Cook C, Mabry L, Reiman MP, Hegedus EJ. Best tests/clinical findings for screening and diagnosis of patellofemoral pain syndrome: a systematic review. Physiotherapy. 2012 Jun 1;98(2):93-100. Link
36. Capin JJ, Snyder-Mackler L. The current management of patients with patellofemoral pain from the physical therapist’s perspective. Annals of joint. 2018 May;3. Link
37. Crossley KM, van Middelkoop M, Callaghan MJ, Collins NJ, Rathleff MS, Barton CJ. 2016 Patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester. Part 2: recommended physical interventions (exercise, taping, bracing, foot orthoses and combined interventions). British journal of sports medicine. 2016 Jul 1;50(14):844-52. Link
38. Walli O, McCay M, Tiu T. Patellofemoral Syndrome: a Review of Diagnosis and Treatment. Current Physical Medicine and Rehabilitation Reports. 2023 Mar 14:1-5. Link
39. Yang X, Yang G, Zuo Y. Whole-body vibration provides additional benefits to patients with patellofemoral pain: A protocol for systematic review and meta analysis of randomized controlled trials. Medicine. 2022 Nov 25;101(47):e31536. Link
40. Giles L, Webster KE, McClelland J, Cook JL. Quadriceps strengthening with and without blood flow restriction in the treatment of patellofemoral pain: a double-blind randomised trial. British journal of sports medicine. 2017 Dec 1;51(23):1688-94. Link
41. Liu Y, Wu L. Effect of instrument-assisted soft tissue mobilization combined with blood flow restriction training on function, pain and strength of patients with patellofemoral joint pain. BMC Musculoskeletal Disorders. 2023 Aug 31;24(1):698. Link
42. Intentionally blank
43. Zago J, Amatuzzi F, Rondinel T, Matheus JP. Osteopathic Manipulative Treatment Versus Exercise Program in Runners With Patellofemoral Pain Syndrome: A Randomized Controlled Trial. Journal of Sport Rehabilitation. 2020 Dec 17;1(aop):1-0. Link
44. Tramontano M, Pagnotta S, Lunghi C, Manzo C, Manzo F, Consolo S, Manzo V. Assessment and management of somatic dysfunctions in patients with patellofemoral pain syndrome. Journal of Osteopathic Medicine. 2020 Mar 1;120(3):165-73. Link
45. Jayaseelan DJ, Scalzitti DA, Palmer G, Immerman A, Courtney CA. The effects of joint mobilization on individuals with patellofemoral pain: A systematic review. Clinical rehabilitation. 2018 Jun;32(6):722-33. Link
46. Motealleh A, Barzegar A, Abbasi L. The immediate effect of lumbopelvic manipulation on knee pain, knee position sense and balance in patients with patellofemoral pain: a randomized controlled trial. Journal of Bodywork and Movement Therapies. 2020 Feb 6. Link
47. Ma YT, Dong YL, Wang B, Xie WP, Huang QM, Zheng YJ. Dry needling on latent and active myofascial trigger points versus oral diclofenac in patients with knee osteoarthritis: a randomized controlled trial. BMC Musculoskeletal Disorders. 2023 Jan 18;24(1):36. Link
48. Crossley K, Cowan SM, Bennell KL, McConnell J. Patellar taping: is clinical success supported by scientific evidence?. Manual therapy. 2000 Aug 1;5(3):142-50. Link
49. Aminaka N, Gribble PA. Patellar taping, patellofemoral pain syndrome, lower extremity kinematics, and dynamic postural control. Journal of athletic training. 2008 Jan 1;43(1):21-8. Link
50. Ho KY, Epstein R, Garcia R, Riley N, Lee SP, Turner C. Effects of patellofemoral taping on patellofemoral joint alignment and contact area during weight bearing. Journal of orthopaedic & sports physical therapy. 2017 Feb;47(2):115-23. Link
51. Edmonds DW, McConnell J, Ebert JR, Ackland TR, Donnelly CJ. Biomechanical, neuromuscular and knee pain effects following therapeutic knee taping among patients with knee osteoarthritis during walking gait. Clinical biomechanics. 2016 Nov 1;39:38-43. Link
52. Collins NJ, Bisset LM, Crossley KM, Vicenzino B. Efficacy of nonsurgical interventions for anterior knee pain: systematic review and meta-analysis of randomized trials. Sports medicine. 2012 Jan;42:31-49. Link
53. Crossley KM, Callaghan MJ, van Linschoten R. Patellofemoral pain. British journal of sports medicine. 2016 Feb 1;50(4):247-50. Link
54. Fukuda TY, Melo WP, Zaffalon BM, Rossetto FM, Magalhães E, Bryk FF, Martin RL. Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up. Journal of orthopaedic & sports physical therapy. 2012 Oct;42(10):823-30. Link
55. Chen Z, Wu J, Wang X, Ren Z. The effect of foot orthoses for patients with patellofemoral pain syndrome: A systematic review and meta-analysis. Heliyon. 2022 Jun 6:e09656. Link
56. Martimbianco AL, Torloni MR, Andriolo BN, Porfírio GJ, Riera R. Neuromuscular electrical stimulation (NMES) for patellofemoral pain syndrome. Cochrane Database of Systematic Reviews. 2017(12). Link
57.de F. Silva A, Maia LB, Mendonça VA, Dos Santos JM, Coelho-Oliveira AC, Santos JN, Moreira LL, Mascarenhas RD, Gonçalves GT, Oliveira VC, Teixeira LA. Efficacy of Hip Strengthening on Pain Intensity, Disability, and Strength in Musculoskeletal Conditions of the Trunk and Lower Limbs: A Systematic Review with Meta-Analysis and Grade Recommendations. Diagnostics. 2022 Nov 23;12(12):2910. Link
58. Khayambashi K, Mohammadkhani Z, Ghaznavi K, Lyle MA, Powers CM. The effects of isolated hip abductor and external rotator muscle strengthening on pain, health status, and hip strength in females with patellofemoral pain: a randomized controlled trial. journal of orthopaedic & sports physical therapy. 2012 Jan;42(1):22-9. Link
59. Nakagawa TH, Muniz TB, Baldon RD, Dias Maciel C, de Menezes Reiff RB, Serrão FV. The effect of additional strengthening of hip abductor and lateral rotator muscles in patellofemoral pain syndrome: a randomized controlled pilot study. Clinical rehabilitation. 2008 Dec;22(12):1051-60. Link
60. Rogan S, Haehni M, Luijckx E, Dealer J, Reuteler S, Taeymans J. Effects of hip abductor muscles exercises on pain and function in patients with Patellofemoral pain: a systematic review and meta-analysis. The Journal of Strength & Conditioning Research. 2019 Nov 1;33(11):3174-87. Link
61. 100. Selkowitz DM, Beneck GJ, Powers CM. Persons with patellofemoral pain exhibit altered hip abductor muscle recruitment while performing hip abductor exercises. Physiotherapy Theory and Practice. 2022 Jul 27:1-0. Link
62. Alammari A, Spence N, Narayan A, Karnad SD, Ottayil ZC. Effect of Hip Abductors and Lateral Rotators Muscle Strengthening on Pain and Functional Outcome in Patients with Patellofemoral Pain: Systematic Review and Meta-Analysis. Link
63. Abd Elrahman AC, Azzam AH, Mohamed NA. Identifying female responders to proximal control exercises in patellofemoral pain syndrome: A clinical prediction rule. Journal of Taibah University Medical Sciences. 2022;17(6):954e961. Link
64. Hossein HS, Sara A, Hasan D. The effect of three types of exercises programs on the patella location in athletes with patellofemoral pain. The Knee. 2023 Mar 1;41:97-105. Link
65. Xie P, István B, Liang M. The Relationship between Patellofemoral Pain Syndrome and Hip Biomechanics: A Systematic Review with Meta-Analysis. InHealthcare 2022 Dec 28 (Vol. 11, No. 1, p. 99). MDPI. Link
66. Bramah C, Preece SJ, Gill N, Herrington L. A 10% Increase in Step Rate Improves Running Kinematics and Clinical Outcomes in Runners With Patellofemoral Pain at 4 Weeks and 3 Months. The American journal of sports medicine. 2019 Oct 28:0363546519879693. Link
67. Bonacci J, Fox A, Hall M, Fuller JT, Vicenzino B. Footwear and Cadence Affect Gait Variability in Runners with Patellofemoral Pain. Medicine and science in sports and exercise. 2020 Feb 5. Link
68. Bonacci J, Fox A, Hall M, Fuller JT, Vicenzino B. Effect of gait retraining on segment coordination and joint variability in individuals with patellofemoral pain. Clinical Biomechanics. 2020 Sep 20:105179. Link
69. Culvenor AG, van Middelkoop M, Macri EM, Crossley KM. Is patellofemoral pain preventable? A systematic review and meta-analysis of randomised controlled trials. British Journal of Sports Medicine. 2020 Oct 28. Link
70. Doyle EW, Doyle TL, Bonacci J, Beach AJ, Fuller JT. Cumulative patellofemoral force and stress are lower during faster running compared to slower running in recreational runners. Sports Biomechanics. 2023 Jun 28:1-3. Link
71. Zhang M, Zhou X, Zhang L, Liu H, Yu B. The effect of heel-to-toe drop of running shoes on patellofemoral joint stress during running. Gait & Posture. 2022 Feb 13. Link
72. Zhang M, Zhou X, Zhang L, Liu H, Yu B. The effect of heel-to-toe drop of running shoes on patellofemoral joint stress during running. Gait & Posture. 2022 Feb 13. Link
73. Nielsen RØ, Parner ET, Nohr EA, Sørensen H, Lind M, Rasmussen S. Excessive progression in weekly running distance and risk of running-related injuries: an association which varies according to type of injury. journal of orthopaedic & sports physical therapy. 2014 Oct;44(10):739-47. Link
74. Rathleff MS, Petersen KK, Arendt-Nielsen L, Thorborg K, Graven-Nielsen T. Impaired conditioned pain modulation in young female adults with long-standing patellofemoral pain: a single blinded cross-sectional study. Pain Medicine. 2016 May 1;17(5):980-8. Link
75. Noehren B, Shuping L, Jones A, Akers DA, Bush HM, Sluka KA. Somatosensory and biomechanical abnormalities in females with patellofemoral pain. The Clinical journal of pain. 2016 Oct;32(10):915. Link
76. Rathleff MS, Roos EM, Olesen JL, Rasmussen S, Arendt-Nielsen L. Lower mechanical pressure pain thresholds in female adolescents with patellofemoral pain syndrome. journal of orthopaedic & sports physical therapy. 2013 Jun;43(6):414-21. Link
77. Maclachlan LR, Collins NJ, Matthews ML, Hodges PW, Vicenzino B. The psychological features of patellofemoral pain: a systematic review. British journal of sports medicine. 2017 May 1;51(9):732-42. Link
78. Chen Z, Wu J, Wang X, Ren Z. The effect of foot orthoses for patients with patellofemoral pain syndrome: A systematic review and meta-analysis. Heliyon. 2022 Jun 6:e09656. Link
79. Kellish AS, Kellish P, Hakim A, Miskiel S, Shahi A, Kellish A. What is the effect on kinesio taping on pain and gait in patients with patellofemoral pain syndrome?. Cureus. 2020 Jul 3;12(7). Link
80. Günay E, Sarıkaya S, Özdolap Ş, Büyükuysal Ç. Effectiveness of the kinesiotaping in the patellofemoral pain syndrome. Turkish Journal of Physical Medicine and Rehabilitation. 2017 Dec;63(4):299. Link
81. Ho KY, Epstein R, Garcia R, Riley N, Lee SP, Turner C. Effects of patellofemoral taping on patellofemoral joint alignment and contact area during weight bearing. Journal of orthopaedic & sports physical therapy. 2017 Feb;47(2):115-23. Link