Joint Cavitation: Does it Matter?
Reading time: 6 minutes
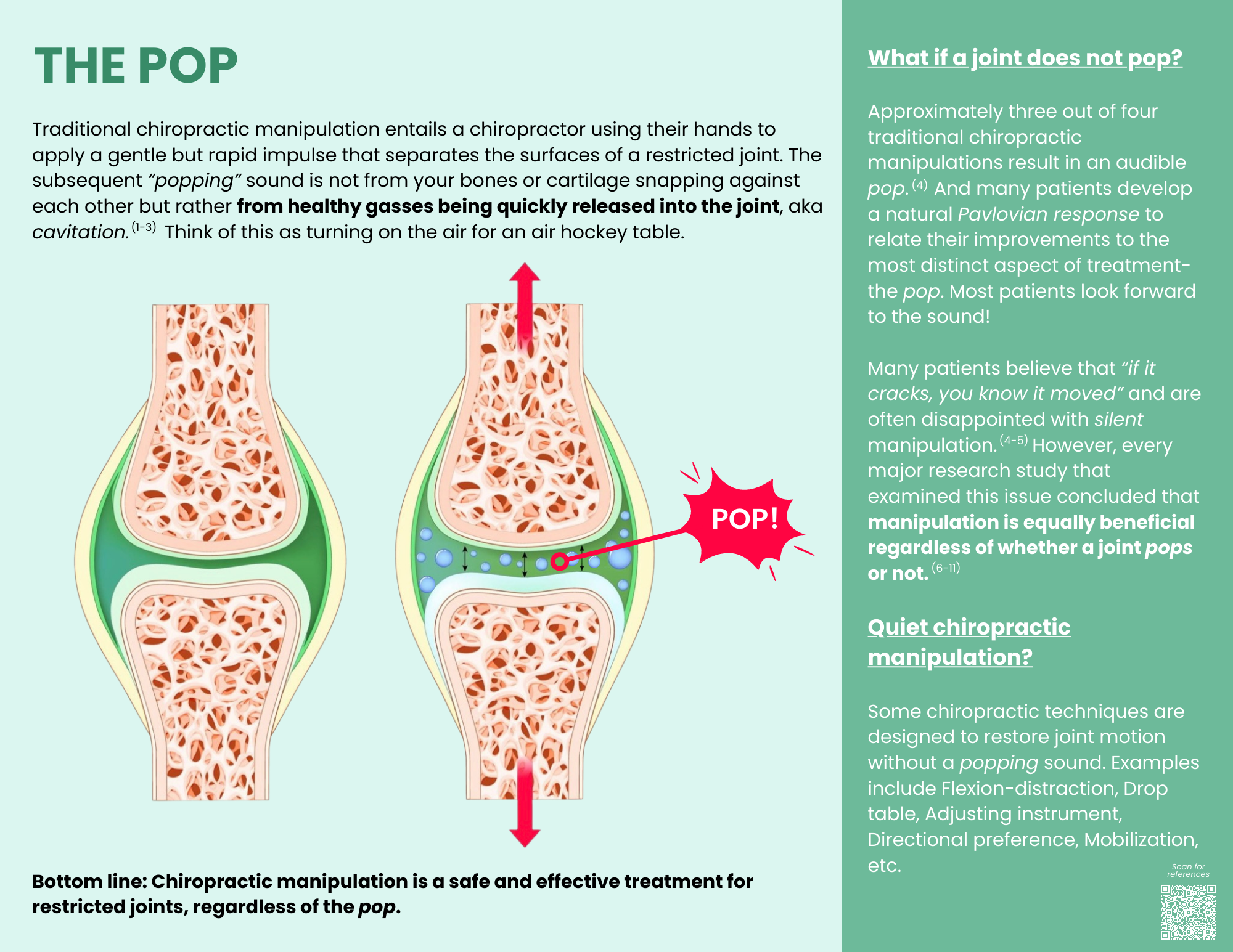
Studies have shown that the audible cavitation of the joints during manipulation doesn't actually impact treatment outcomes. However, a patient’s expectations of hearing a pop can contribute positively toward improved outcomes… or negatively via a nocebo effect.
This means patient education is key. This blog will equip you with evidence-based answers to the top five questions, plus a downloadable patient infographic to help explain joint manipulation and manage patient expectations around the “pop.”
1. What causes joint cavitation?
Short answer: The science is not definitive, but probably the distraction-induced release of gasses within the joint fluid, aka “tribonucleation.” (1)
Deeper dive: The specific mechanism(s) of audible joint cavitation remain undefined.
“High-velocity, low-amplitude thrust manipulation consists of applying a rapid impulse accompanied by an audible pop sound. The exact origin of the popping sound is still unknown and under debate.” (2)
As mentioned in the What is Manipulation blog by the other guy 😏, the three leading hypotheses include:
Creation of vapor bubbles via rapid separation of joint surfaces, aka “tribonucleation.”(1,3,4) Essentially, quickly lowering the pressure on a fluid allows dissolved gasses to escape and coalesce.
The collapse of vapor bubbles (5-7)
Multiple concurrent mechanisms (8-10)
One prevailing premise suggests sound is created by “rapid separation of the joint surfaces with subsequent gas cavity formation.” (1,2,4,11)
“When sufficient distraction force overcomes the viscous attraction or adhesive forces between opposing joint surfaces, rapid separation of the articulation occurs with the resulting drop in synovial pressure allowing dissolved gas to come out of solution to form a cavity within the joint. This cavity persists after the popping sound is produced and therefore proposes that joint cracking is associated with cavity formation within the synovial fluid.” (11)
2. Provider beliefs: Does joint cavitation matter?
Short answer: It probably depends on how often you “pop” joints.
Deeper dive: This might be hard to imagine, but not all chiropractors agree about the significance of a “pop.” 🤯
“There is still no consensus among chiropractors on the association of an audible pop and pain outcomes in spinal manipulative therapy.” (11)
Many HVLA-oriented manual therapists believe that a popping sound is a primary differentiator between manipulation and mobilization. (11,12) Several sources suggest that an audible popping sound is a primary characteristic of successful joint manipulation. (2,13,21) In fact, many providers apply subsequent thrusts if the first (or second, or third…) attempt did not result in an audible release. (11,22)
One recent literature analysis, including five studies of 303 patients, determined that approximately three out of four (74%) manipulations resulted in audible joint cavitation. (11) Other authors have shown that the frequency of audible joint cavitation increases with experience and speed. (23,24)
Thus, the natural Pavlovian response would persuade HVLA chiropractors to mentally connect incremental improvements in audible joint cavitation and treatment success.
3. Patient beliefs: Does joint cavitation matter?
Short answer: “If it cracks, you know it has moved”
Deeper dive: Like providers, patients also have a natural Pavlovian response to relate their improvements to the most distinct aspect of care - audible joint cavitation. In fact, experienced providers will attest to many stories of patients who sighed with relief when the provider's knuckles cavitated as they motion palpated or thrust on the patient.
Multiple studies have concluded that most patients believe the absence of a popping sound equates to an ineffective thrust manipulation. (2,25,26) One study suggested that 75% of patients believe that “If it cracks, you know it has moved” and that a popping sound is essential. (26)
However, patient and provider expectations may not align with the current literature.
4. What does the research say about joint cavitation?
Short answer: The pop does not matter
Deeper dive: Multiple studies have shown no difference in range of motion, pain, or disability outcomes between thrust manipulation with and without associated audible cavitation. (27-31) One recent review of five prior studies concluded: “regardless of the area of the spine manipulated or follow-up time, there was no evidence of improved pain outcomes associated with an audible pop.” (11)
5. Do chiropractors need joint cavitation patient education?
Short answer: Yes. The nocebo effect is in play when patients expect a “pop” but don’t experience it.
The Nocebo Effect
“The opposite of the placebo effect. It describes a situation where a negative outcome occurs due to a belief that the intervention will [not work or] cause harm. Some experts state that the nocebo effect may have a larger effect on clinical outcomes than the placebo effect as negative perceptions are formed much faster than positive one.” (32)
Deeper dive: Evidence-based providers understand that a patient’s biopsychosocial perspective regarding manipulation can dramatically impact compliance, outcomes, and chronicity. (2,33)
“Inconsistency between patient beliefs for understanding the popping sound after thrust manipulation and the explanations currently provided can potentially alter patient-reported outcome changes.” (25)
Patients often mistakenly believe that their healing is dependent on the provider. (34) These same patients are subject to a potent nocebo effect if they also believe that successful therapy requires the provider to deliver a “pop.” (2,25)
“Practitioners who perform thrust manipulation should pay attention to patients' beliefs and clearly explain the aim and effectiveness of thrust manipulation using current theoretical models.” (2)
One recent study found that nearly one-third (31%) of HVLA patients did not recall receiving any information on the mechanisms or effects of manipulation. (2) Educating and preparing patients' expectations for HVLA can help mitigate the nocebo effect, leading to better outcomes and compliance. (2,34,35)
Good news for you! Your ChiroUp team has created an informative infographic to help you educate patients and avoid the nocebo effect. Subscribers can access the infographic in the Forms Library by searching “The Pop”.
Want to navigate your day-to-day practice with ease?
Be confident that you are giving your patients the highest standard of care based on the latest evidence-based chiropractic research with Chiroup. Join our network for FREE today and start practicing with confidence!
-
1. Kawchuk GN, Fryer J, Jaremko JL, Zeng H, Rowe L, Thompson R. Real-time visualization of joint cavitation. PloS one. 2015 Apr 15;10(4):e0119470. Link
2. Bergamino M, Vongher A, Mourad F, Dunning J, Rossettini G, Palladino M, Fernández-de-Las-Peñas C, Testa M, Maselli F. Patient concerns and beliefs related to audible popping sound and the effectiveness of manipulation: findings from an online survey. Journal of Manipulative and Physiological Therapeutics. 2022 Feb 1;45(2):144-52. Link
3. Roston JB, Haines RW. Cracking in the metacarpo-phalangeal joint. Journal of anatomy. 1947 Apr;81(Pt 2):165. Link
4. Brodeur R. The audible release associated with joint manipulation. Journal of manipulative and physiological therapeutics. 1995 Mar 1;18(3):155-64. Link
5. Unsworth A, Dowson D, Wright V. 'Cracking joints'. A bioengineering study of cavitation in the metacarpophalangeal joint. Annals of the rheumatic diseases. 1971 Jul;30(4):348. Link
6. Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for acute low‐back pain. Cochrane Database of Systematic Reviews. 2012(9). Link
7. Chandran Suja V, Barakat AI. A mathematical model for the sounds produced by Knuckle cracking. Scientific Reports. 2018 Mar 29;8(1):1-9. Link
8. Dunning J, Mourad F, Zingoni A, Iorio R, Perreault T, Zacharko N, de Las Peñas CF, Butts R, Cleland JA. Cavitation sounds during cervicothoracic spinal manipulation. International Journal of Sports Physical Therapy. 2017 Aug;12(4):642. Link
9. Mourad F, Dunning J, Zingoni A, Iorio R, Butts R, Zacharko N, Fernández-de-Las-Peñas C. Unilateral and multiple cavitation sounds during lumbosacral spinal manipulation. Journal of Manipulative and Physiological Therapeutics. 2019 Jan 1;42(1):12-22. Link
10. Dunning J, Mourad F, Barbero M, Leoni D, Cescon C, Butts R. Bilateral and multiple cavitation sounds during upper cervical thrust manipulation. BMC musculoskeletal disorders. 2013 Dec;14:1-2. Link
11. Moorman AC, Newell D. Impact of audible pops associated with spinal manipulation on perceived pain: a systematic review. Chiropractic & manual therapies. 2022 Dec;30(1):1-1. Link
12. Evans DW, Breen AC. A biomechanical model for mechanically efficient cavitation production during spinal manipulation: prethrust position and the neutral zone. Journal of Manipulative & Physiological Therapeutics. 2006 Jan 1;29(1):72-82. Link
13. Cramer GD, Ross JK, Raju PK, Cambron JA, Dexheimer JM, Bora P, McKinnis R, Selby S, Habeck AR. Distribution of cavitations as identified with accelerometry during lumbar spinal manipulation. Journal of manipulative and physiological therapeutics. 2011 Nov 1;34(9):572-83. Link
14. Herzog W, Zhang YT, Conway PJ, Kawchuk GN. Cavitation sounds during spinal manipulative treatments. Journal of manipulative and physiological therapeutics. 1993 Oct;16(8):523-6. Link
15. Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific?. Spine. 2004 Jul 1;29(13):1452-7. Link
16. Triano JJ. Studies on the biomechanical effect of a spinal adjustment. Journal of manipulative and physiological therapeutics. 1992 Jan 1;15(1):71-5. Link
17. Intentionally blank
18. González-Iglesias J, Fernández-de-las-Peñas C, Cleland JA, Alburquerque-Sendín F, Palomeque-del-Cerro L, Méndez-Sánchez R. Inclusion of thoracic spine thrust manipulation into an electro-therapy/thermal program for the management of patients with acute mechanical neck pain: a randomized clinical trial. Manual therapy. 2009 Jun 1;14(3):306-13. Link
19. González-Iglesias J, Fernandez-De-Las-Penas C, Cleland JA, del Rosario Gutiérrez-Vega M. Thoracic spine manipulation for the management of patients with neck pain: a randomized clinical trial. Journal of orthopaedic & sports physical therapy. 2009 Jan;39(1):20-7. Link
20. Dunning JR, Cleland JA, Waldrop MA, Arnot C, Young I, Turner M, Sigurdsson G. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. journal of orthopaedic & sports physical therapy. 2012 Jan;42(1):5-18. Link
21. Evans DW, Lucas N. What is ‘manipulation’? A reappraisal. Manual therapy. 2010 Jun 1;15(3):286-91. Link
22. Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific?. Spine. 2004 Jul 1;29(13):1452-7. Link
23. Van Geyt B, Dugailly PM, Klein P, Lepers Y, Beyer B, Feipel V. Assessment of in vivo 3D kinematics of cervical spine manipulation: influence of practitioner experience and occurrence of cavitation noise. Musculoskeletal Science and Practice. 2017 Apr 1;28:18-24. Link
24. Williams JM, Cuesta-Vargas A. Quantification of Prone Thoracic Manipulation Using Inertial Sensor–Derived Accelerations. Journal of Manipulative and Physiological Therapeutics. 2014 May 1;37(4):230-5. Link
25. Demoulin C, Baeri D, Toussaint G, Cagnie B, Beernaert A, Kaux JF, Vanderthommen M. Beliefs in the population about cracking sounds produced during spinal manipulation. Joint Bone Spine. 2018 Mar 1;85(2):239-42. Link
26. Miller PJ, Poggetti AS. Qualitative study on chiropractic patients’ personal perception of the audible release and cavitation. Clinical Chiropractic. 2011 Mar 1;14(1):8-16. Link
27. Flynn TW, Fritz JM, Wainner RS, Whitman JM. The audible pop is not necessary for successful spinal high-velocity thrust manipulation in individuals with low back pain. Archives of physical medicine and rehabilitation. 2003 Jul 1;84(7):1057-60. Link
28. Bialosky JE, Bishop MD, Robinson ME, George SZ. The relationship of the audible pop to hypoalgesia associated with high-velocity, low-amplitude thrust manipulation: a secondary analysis of an experimental study in pain-free participants. Journal of manipulative and physiological therapeutics. 2010 Feb 1;33(2):117-24. Link
29. Sillevis R, Cleland J. Immediate effects of the audible pop from a thoracic spine thrust manipulation on the autonomic nervous system and pain: a secondary analysis of a randomized clinical trial. Journal of manipulative and physiological therapeutics. 2011 Jan 1;34(1):37-45. Link
30. Cleland JA, Flynn TW, Childs JD, Eberhart S. The audible pop from thoracic spine thrust manipulation and its relation to short-term outcomes in patients with neck pain. Journal of manual & manipulative therapy. 2007 Jul 1;15(3):143-54. Link
31. Flynn TW, Childs JD, Fritz JM. The audible pop from high-velocity thrust manipulation and outcome in individuals with low back pain. Journal of manipulative and physiological therapeutics. 2006 Jan 1;29(1):40-5. Link
32. Medsafe. The Nocebo Effect. Prescriber Update 40(1): 14–15. March 2019 Link
33. Funabashi M, Pohlman KA, Goldsworthy R, Lee A, Tibbles A, Mior S, Kawchuk G. Beliefs, perceptions and practices of chiropractors and patients about mitigation strategies for benign adverse events after spinal manipulation therapy. Chiropractic & Manual Therapies. 2020 Dec;28(1):1-9. Link
34. Demoulin C, Roussel N, Marty M, Mathy C, Genevay S, Henrotin Y, Tomasella M, Mahieu G, Vanderthommen M. The maladaptive beliefs of patients with low back pain. A narrative review. Revue Medicale de Liege. 2016 Jan 1;71(1):40-6. Link
35. Rossettini G, Colombi A, Carlino E, Manoni M, Mirandola M, Polli A, Camerone EM, Testa M. Unraveling negative expectations and nocebo-related effects in musculoskeletal pain. Frontiers in Psychology. 2022:1184. Link