Essential Skills To Resolve Cluneal Neuropathy
Reading time: 5 minutes
According to the most recent ChiroUp Clinical Outcomes and Patient Satisfaction Synopsis of more than 630,000 unique presentations, lumbosacral pain is the most common complaint in chiropractic practices.
Fortunately, most low back and buttock pain presentations are straightforward diagnoses that respond quickly and favorably to chiropractic management. But… 😏those elusive few presentations that fail our care are the ones that keep us awake at night.
Lucky for you, ChiroUp is on a mission to help you sleep well as an Expert Clinician armed with the latest skills to confidently resolve problems. So this blog will cover one of the most overlooked causes of lumbosacral and buttock pain, as noted last month in the Journal of General and Family Medicine (1):
“Cluneal nerve entrapment syndrome is often overlooked and misdiagnosed.”
And if a PCP can recognize an unusual mechanical LBP diagnosis, you should be a master at managing it; in the next 3 minutes, you’ll learn the essential cluneal neuropathy clinical skills to help ensure you won’t overlook or misdiagnose this condition ever again.
What Is Cluneal Neuropathy?
Quick answer: Irritation or entrapment of the superior cluneal nerves
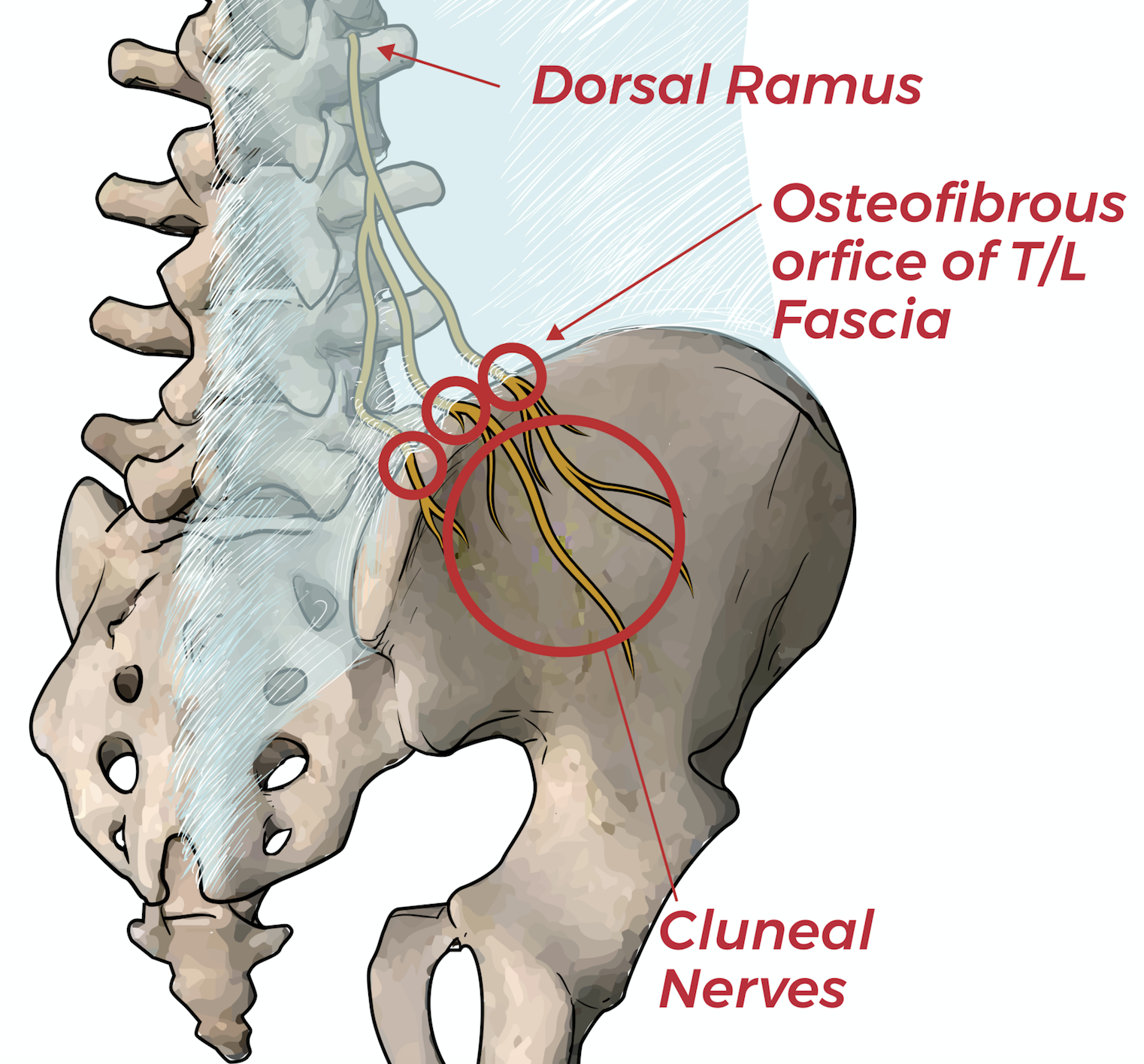
Cluneal neuropathy describes entrapment of the superior cluneal nerves at the iliac crest. The cluneal nerve originates from the thoracolumbar dorsal rami then diverges inferiorly into branches that surface through osteofibrous tunnels over the iliac crest, approximately 4 and 8 cm from midline.
Entrapment often occurs at the osteofibrous orifice where the nerves penetrate the thoracolumbar fascia before innervating the cutaneous regions of the iliac crest and buttock. (5-8) These distal entrapments can increase neurodynamic tension on the dorsal nerve root, thereby generating ischemia and hyperexcitability. (7,8) Compression or irritation results in radiating pain or paresthesia into the lumbosacral spine, hip, or buttock.
How Does Cluleal Neuropathy Differ From Maigne Syndrome?
Quick answer: Peripheral vs proximal nerve irritation
Any reference to cluneal nerve entrapment would be incomplete without a discussion of Maigne syndrome; however, those diagnoses are not synonymous. Maigne syndrome involves irritation of the dorsal root near the spine, while cluneal nerve entrapment is a more peripheral neuropathy. The relationship could be likened to cervical radiculopathy and carpal tunnel syndrome, respectively. And the conditions frequently co-exist as double crush partners. Check out ChiroUp to learn how.
Who Gets Cluneal Neuropathy?
Short answer: A S#!t ton more patients than you would expect
Cluneal nerve irritation (including Maigne syndrome) may be a causative or contributory factor in up to 40% of LBP cases. (5,40,41) That prospect increases as symptoms extend over the posterior iliac crest. (2) Cluneal nerve entrapment can affect any age group but is most common in the 55-70-year-old population, and seems to have a slight preference for females. (40)
What Are The Symptoms Of Cluneal Neuropathy?
Short answer: It looks and smells like typical mechanical lumbosacral dysfunction
The most common manifestation of superior cluneal nerve irritation is low back pain that mirrors the presentation of lumbosacral or sacroiliac joint dysfunction. (3,9) Symptoms including pain, numbness, or paresthesia characteristically refer to the lumbosacral region, iliac crest, or groin. (7,9-12) Symptoms are typically described as chronic, constant, and unilateral, although the problem could present on both sides concurrently. (3,40).
Cluneal nerve entrapment can be exacerbated by transitional movements, like arising from a seated position, rolling in bed, squatting, lateral bending, and trunk rotation. (8,40) Prolonged walking is also a known trigger for cluneal nerve irritation. (8,12,14)
What Tests Can Help Diagnose Cluneal Neuropathy?
Short answer: Poke, pinch, or tap the nerve
In cases of peripheral cluneal nerve entrapment, patients will often report palpatory tenderness at the primary site of entrapment on the posterior iliac crest, approximately 3–4 cm (medial branch) or 7–8 cm (intermediate/ middle branch) from the midline. (8,12,40) Pinching or skin rolling may demonstrate hyperalgesia over the flank and iliac crest. (10,14,17)
A thickening of tissue over the posterior rim of the iliac crest has been reported in some cases. (28) Tapping a reflex hammer over the entrapped nerve may reproduce symptoms, including a shock-like sensation (Tinel’s sign) (28)
How Do I Treat Cluneal Neuropathy?
Short answer: Cluneal nerve release, manipulation, and rehab
Cluneal nerve entrapment and Maigne syndrome can be frustrating conditions to manage for both patients and clinicians. (3,28) The long-term treatment goals include restoring biomechanical function at the thoracolumbar junction and reestablishing normal peripheral neurodynamics.
Modalities
Electrical stimulation and ice might help decrease pain and inflammation in the early stages. (18)
Manipulation
Dr. Maigne identified “painful minor intervertebral dysfunction” as a common finding in his namesake condition. (3) Not surprisingly, spinal manipulation of the thoracolumbar junction appears to provide benefit. (13,16,35). Manipulation and mobilization should also address any other joint restrictions throughout the kinetic chain, particularly in the lumbar, sacral, thoracic, and costovertebral regions. Some experts advocate for the use of a foam roller to further enhance mobility at home. (36)
Cluneal Nerve Release
Excessive fascial tightness can generate traction ischemia and hyperexcitability of the dorsal nerve root. (33) Myofascial release may help improve fascial movement and pliability in patients with chronic back pain. (34) Myofascial release should focus on the thoracolumbar aponeurosis and distribution of the cluneal nerve (16,18) IASTM could be a management consideration. (16)
Rehab
Flexibility exercises should target the thoracolumbar erectors and iliopsoas, particularly if the patient has adopted a compensatory flexed posture. Stretching could include a standing hip flexor stretch, half-kneeling psoas stretch, and progressive latissimus stretches. Spinal elongation self-correction may also be useful. (45) A progression of pelvic tilt exercises has been advocated for the care of Maigne syndrome. (18)
Early stability rehab could begin with a prone plank and advance to progressive variations. (45) Active rehabilitation should focus on building strength in the hip and core stabilizers. (9,16) Long-term resolution necessitates the restoration of normal breathing mechanics and correction of any other contributory functional deficits.
How Do I Motivate Cluneal Neuropathy Patients to Follow My Treatment Plan and Actively Participate?
Short answer: Four clicks
We’re glad you asked because we made this one crazy simple. Watch this 1-minute video to learn how.
Like what you see? Create reports like these in less than 4 clicks for your patients! Our subscribers have greater than 80% average improvement within 30 days. Sounds amazing, right!? Get started with ChiroUp today to start seeing results like this.
-
1. Mizumoto J. Superior cluneal nerve entrapment syndrome: a common but often overlooked cause of low back pain. Journal of General and Family Medicine. 2022 May;23(3):183-4. Link
2. Kim SR, Lee MJ, Lee SJ, Suh YS, Kim DH, Hong JH. Thoracolumbar junction syndrome causing pain around posterior iliac crest: a case report. Korean journal of family medicine. 2013 Mar;34(2):152. Link
3. Cain L. Maigne’s Syndrome. HFE Health and Fitness Education. 2020 Jan 14. Link
4. Proctor D, Dupuis P, Cassidy JD. Thoracolumbar syndrome as a cause of low-back pain: a report of two cases. The Journal of the Canadian Chiropractic Association. 1985 Jun;29(2):71. Link
5. Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K, Hokari M, Isobe M, Kusano M. Association between intermittent low-back pain and superior cluneal nerve entrapment neuropathy. Journal of Neurosurgery: Spine. 2016 Feb 1;24(2):263-7. Link
6. Pecina MM, Markiewitz AD, Krmpotic-Nemanic J. Tunnel syndromes. CRC press; 2001 Aug 16.
7. Noh K, Jung JB, Seong JW, Kim DE, Kwon D, Kim Y. Thoracolumbar Junction Syndrome Accompanying Renal Artery Stenosis: A Case Report. Annals of Rehabilitation Medicine. 2020 Feb 29;44(1):85-9. Link
8. Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K, Hokari M, Isobe M, Kusano M. Association between intermittent low-back pain and superior cluneal nerve entrapment neuropathy. Journal of Neurosurgery: Spine. 2016 Feb 1;24(2):263-7. Link
9. Maigne R. Low back pain of thoracolumbar origin (T11-T12-L1). Diagnosis and treatment of pain of vertebral origin. 2nd ed. Boca Raton: Tayloe and Francis Group. 2006:289-98.
10. Noh K, Jung JB, Seong JW, Kim DE, Kwon D, Kim Y. Thoracolumbar Junction Syndrome Accompanying Renal Artery Stenosis: A Case Report. Annals of Rehabilitation Medicine. 2020 Feb 29;44(1):85-9. Link
11. Aktas ?, Akgün K, Palamar D, Saridogan M. Thoracolumbar junction syndrome: An overlooked diagnosis in an elderly patient. Turkish Journal of Geriatrics/Türk Geriatri Dergisi. 2014 Apr 1;17(2). Link
12. Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, Butler B, Garber M, Allison S. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002 Dec 15;27(24):2835-43. Link
13. Aoun F, Malek E, Kazan D, Albisinni S, Peltier A, Bollens R, Roumeguère T. Management of chronic testicular pain due to thoracolumbar junction syndrome: A pilot study. Progrès en Urologie. 2020 Jan 21. Link
14. Alptekin K, Örnek NI, Ayd?n T, Alkan M, Toprak M, Balc? LA, Alptekin JÖ. Effectiveness of exercise and local steroid injections for the thoracolumbar junction syndrome (The Maigne’s syndrome) treatment. The open orthopaedics journal. 2017;11:467.Link
15. Zhou L., Schneck C.D., Shao Z. The anatomy of dorsal ramus nerves and its implications in lower back pain. Neurosci. Med. 2012;3:192–201. doi: 10.4236/nm.2012.32025.
16. DiMond ME. Rehabilitative principles in the management of thoracolumbar syndrome: a case report. Journal of chiropractic medicine. 2017 Dec 1;16(4):331-9. Link
17. Frisch H. Programmierte Untersuchung Des Bewegungsapparates. Berlin: Springer-Verlag; 1983.
18. Alptekin K, Örnek NI, Ayd?n T, Alkan M, Toprak M, Balc? LA, Alptekin JÖ. Effectiveness of exercise and local steroid injections for the thoracolumbar junction syndrome (The Maigne’s syndrome) treatment. The open orthopaedics journal. 2017;11:467. Link
19. Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. International journal of sports physical therapy. 2013 Feb;8(1):62. Link
20. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Archives of physical medicine and rehabilitation. 2005 Sep 1;86(9):1753-62. Link
21. Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Archives of Physical Medicine and Rehabilitation. 2005 Sep 1;86(9):1745-52. Link
22. Liebenson C, Karpowicz AM, Brown SH, Howarth SJ, McGill SM. The active straight leg raise test and lumbar spine stability. PM&R. 2009 Jun 1;1(6):530-5. Link
23. Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Archives of physical medicine and rehabilitation. 2003 Dec 1;84(12):1858-64. Link
24. Nachemson A. Lumbar spine instability. A critical update and symposium summary. Spine. 1985 Apr;10(3):290-1. Link
25. Ogon M, Bender BR, Hooper DM, Spratt KF, Goel VK, Wilder DG, Pope MH. A dynamic approach to spinal instability: Part I: Sensitization of intersegmental motion profiles to motion direction and load condition by instability. Spine. 1997 Dec 15;22(24):2841-58. Link
26. Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Physical therapy. 1995 Jun 1;75(6):470-85. Link
27. Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992 Jun;17(6):617-28. Link
28. Morgan, WE. Cluneal Nerve Entrapment: Lumbo-Pelvic Pain Part 2. Accessed 04/28/20 from: http://drmorgan.info/clinicians-corner/cluneal-nerve-entrapment/
29. Kolá P, Šulc J, Kyn l M, Šanda J, Akrt O, Andel R, Kumagai K, Kobesová A. Postural function of the diaphragm in persons with and without chronic low back pain. Journal of orthopaedic & sports physical therapy. 2012 Apr;42(4):352-62. Link
30. Walker HK, Hall WD, Hurst JW. The Oral Cavity and Associated Structures--Clinical Methods: The History, Physical, and Laboratory Examinations. Butterworths; 1990.
31. Aktas I, Akgun K. Thoracolomber junction syndrome. Bogazici Tip Dergisi. 2014;1(1):29-31.
32. Langevin HM, Fox JR, Koptiuch C, Badger GJ, Greenan-Naumann AC, Bouffard NA, Konofagou EE, Lee WN, Triano JJ, Henry SM. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC musculoskeletal disorders. 2011 Dec 1;12(1):203. Link
33. Seong JW. Principle and insight into pain. Paju, Korea: Koonja Press; 2012. p.844–55.
34. Branchini M, Lopopolo F, Andreoli E, Loreti I, Marchand AM, Stecco A. Fascial Manipulation® for chronic aspecific low back pain: a single blinded randomized controlled trial. F1000Research. 2015;4. Link
35. Kim SR, Lee MJ, Lee SJ, Suh YS, Kim DH, Hong JH. Thoracolumbar junction syndrome causing pain around posterior iliac crest: a case report. Korean journal of family medicine. 2013 Mar;34(2):152. Link
36. Morgan, WE. Maigne's Syndrome: Lumbo-Pelvic Pain Part 1. Accessed 04/28/20 from: http://drmorgan.info/clinicians-corner/maigne-s-syndrome/. Link
37. Maigne R. Diagnosis and treatment of pain of vertebral origin: a manual medicine approach. Baltimore: Williams & Wilkins; 1996.
38. Maigne JY, Doursounian L. Entrapment neuropathy of the medial superior cluneal nerve: Nineteen cases surgically treated, with a minimum of 2 years' follow-up. Spine. 1997 May 15;22(10):1156-9. Link
39. Kuniya H, Aota Y, Kawai T, Kaneko KI, Konno T, Saito T. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. Journal of orthopaedic surgery and research. 2014 Dec;9(1):139. Link
40. Isu T, Kim K, Morimoto D, Iwamoto N. Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain. Neurospine. 2018;15(1):25?32. Link
41. Maigne R. Low back pain of thoracolumbar origin. Archives of physical medicine and rehabilitation. 1980 Sep;61(9):389-95. Link
42. Cui HS, Hong AR, Kim JB, Yu JH, Cho YS, Joo SY, Seo CH. Extracorporeal shock wave therapy alters the expression of fibrosis-related molecules in fibroblast derived from human hypertrophic scar. International journal of molecular sciences. 2018 Jan;19(1):124. Link
43. Mulligan BR. Mobilisations with movement (MWM'S). Journal of Manual & Manipulative Therapy. 1993 Jan 1;1(4):154-6. Link
44. Mulligan BR. Manual Therapy: NAGS, SNAGS, MWM etc. 6th Ed. Plane View Services Ltd. Wellington, NZ. 2010
45. Tucker J. “Maigne Syndrome” Message to Tim Bertelsman regarding advice on chiropractic management of Maigne syndrome patients via direct email on 05/02/2020.
46. Griffiths FS, McSweeney T, Edwards DJ. Immediate effects and associations between interoceptive accuracy and range of motion after a HVLA thrust on the thoracolumbar junction: A randomised controlled trial. Journal of Bodywork and Movement Therapies. 2019 Jun 8. Link
47. Visnjevac O, Pastrak M, Ma F, Visnjevac T, Abd-Elsayed A. Radiofrequency Ablation of the Superior Cluneal Nerve: A Novel Minimally Invasive Approach Adopting Recent Anatomic and Neurosurgical Data. Pain and Therapy. 2022 Apr 17:1-1. Link