Chiropractic Use of Shockwave Therapy
Welcome, fellow chiropractors and evidence-loving clinicians! Today, we’re going to dive into a topic that might just ruffle a few feathers: the idea that shockwave therapy is not a magic wand. That’s right, your beloved shockwave machine won’t solve all the world’s musculoskeletal problems. Shocking, I know!
You’ve probably heard the jokes; some folks think that if you just blast a tendon or muscle with enough shockwaves, you can fix everything from plantar fasciitis to their morning coffee jitters. And don’t get me wrong: shockwave therapy is a fantastic tool. Studies from high-impact journals have demonstrated its effectiveness in treating chronic tendinopathies, bone injuries, and specific nerve-related issues. It's like having a superhero in your toolbox, but even superheroes have their kryptonite.
When Shockwave Isn’t Indicated
So, let’s get into those scenarios where shockwave is not your go-to hero. Here are four prime examples: (1)
1. Open Growth Plates (Physes) in Children
Applying shockwave therapy directly over an open physis (longitudinal growth plate) in children is generally contraindicated. The physis is a highly specialized cartilage structure responsible for bone lengthening and contains fragile proliferative and hypertrophic zones that are vulnerable to mechanical stress.
For this reason, it has historically been listed as a contraindication for shockwave therapy. While recent animal studies suggest that low-energy shockwave does not damage growth plates and may even stimulate growth signaling (2), there are no human clinical trials supporting direct treatment over physes, and long-term safety data are lacking. Accordingly, physeal growth plates should still be protected, and rest and load modification remain the standard of care.
Apophyses Are Different
An apophysis is not a physis. It is a secondary ossification center designed to tolerate traction forces from tendon or ligament attachment, and its fibrocartilaginous, collagen-rich structure is fundamentally different from the delicate cartilage of a physeal growth plate. Multiple human studies now demonstrate that low-energy shockwave therapy applied to apophyseal injuries, such as Osgood-Schlatter disease, Sever’s disease, and Little League elbow, leads to rapid pain relief, a faster return to sports, and no observed growth disturbance, even at long-term follow-up. (3-5) These treatments used low-energy protocols and typically targeted the surrounding tissues rather than the apophyseal cartilage itself.
Notably, the recent international Delphi consensus panel did not provide a clear green light or red light for the use of shockwaves near open epiphyseal plates, as expert agreement varied. (1) Therefore, clinicians should rely on case-by-case judgment, use low-energy protocols, and monitor patients closely, even as emerging clinical studies suggest that treatment around traction apophyses may be acceptable.
2. Active Infections or Tumors
If there’s an infection or any kind of malignancy, step away from the shockwave. We don’t want to stimulate anything that shouldn't be stimulated.
3. Clotting Disorders or Anticoagulant Therapy
If someone is on blood thinners and undergoes shockwave therapy, the primary concern is excessive bleeding into the tissues. Shockwave works by delivering mechanical pressure that intentionally stresses tissue, and when the blood’s ability to clot is reduced, that stress can lead to unwanted side effects, including:
Excessive bruising or hematoma formation under the skin or within a muscle.
Prolonged soreness or swelling that lasts longer than expected.
Localized bleeding that may not be immediately visible but can increase pain or delay recovery.
Delayed healing response, because regular tissue repair relies in part on controlled inflammation and clot formation.
4. Severe Vascular or Nerve Disorders
If there’s severe vascular disease or significant neurologic compromise, shockwave therapy has traditionally been considered a contraindication or strong precaution, largely out of concern for tissue vulnerability and the potential to aggravate impaired perfusion or nerve function.
That said, this is an area worth keeping an eye on. The evidence base for certain “neurovascular” conditions (including subsets of diabetic neuropathy) is evolving, and some studies suggest potential benefit in carefully selected patients. As the research matures, clinical decision-making can evolve with it, but for now, most clinicians should still treat severe vascular or neurologic disorders as a relative red-flag category, using judgment, patient selection, and appropriate precautions. (6-8)
My Favorite Use: Gluteal Tendinopathy
Now that I’ve listed the conditions for which shockwave is not indicated, let’s discuss one of my favorite uses for it: Gluteal Tendinopathy. In my clinic, I’ve seen fantastic results using shockwave therapy on patients with stubborn gluteal tendon issues. It’s not just about the shockwave, of course: we combine it with manual therapy, manipulation, and correcting any functional imbalances that led to the issue in the first place. But shockwave is a great way to kickstart these patients’ road to recovery. It’s like giving their healing process a little turbo boost.
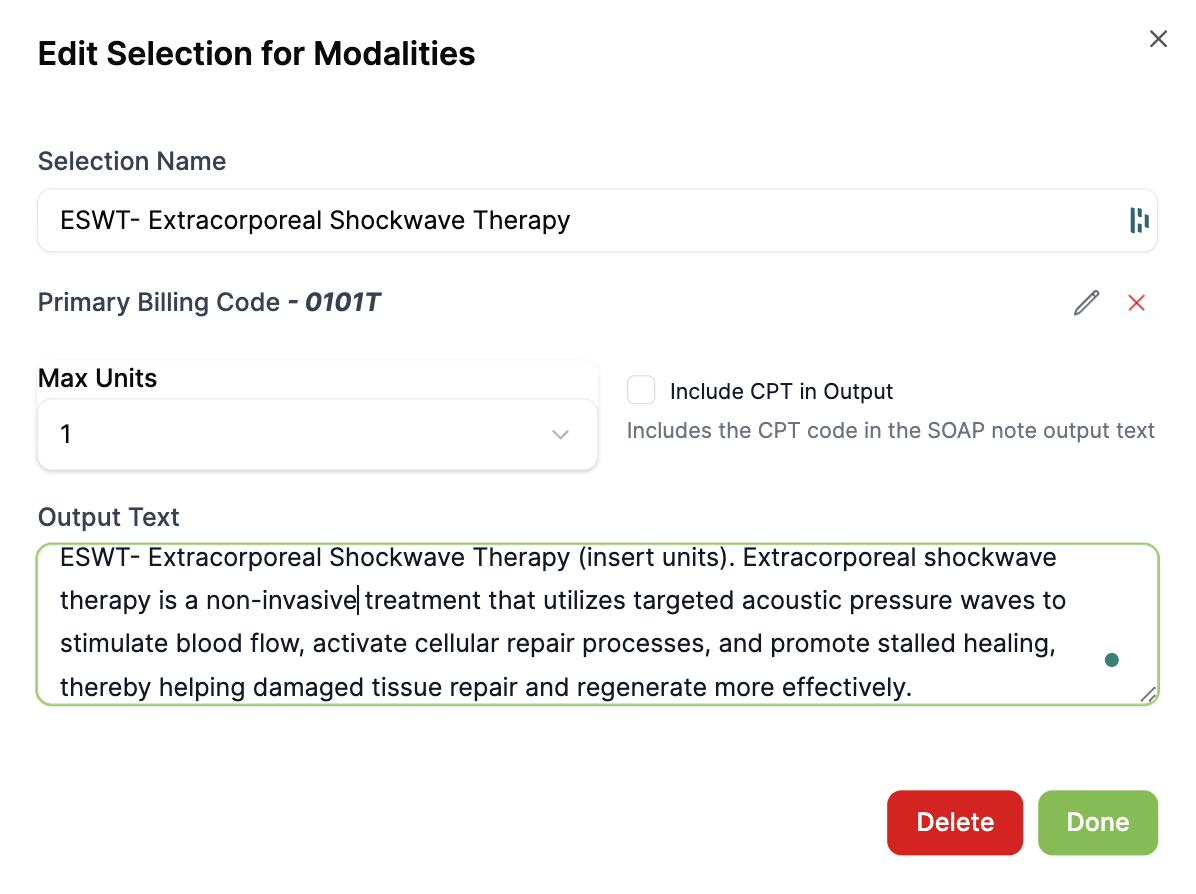
I have been using Shockwave extensively over the last several months, so I have added a new button to my plan section in the EHR to bill for shockwave and include a description in my SOAP note. Check it out in your User Settings.
Chiropractic Use of Shockwave
Shockwave therapy is a powerful and effective tool when used in the right clinical scenarios, with a substantial body of research from respected journals supporting its use for conditions such as chronic tendinopathies and plantar fasciitis. Our research team continually reviews and adds new evidence each month, now supporting the use of shockwave across more than 150 conditions. As an evidence-based chiropractor, be sure to reference the Condition Reference section in ChiroUp for the specific conditions you treat to confirm when shockwave is indicated. When applied thoughtfully, it’s an excellent addition to your clinical toolkit: just remember it’s not a one-size-fits-all solution: use it where the evidence supports it, and avoid it where it doesn’t.
In fact, a recent Delphi analysis revealed that this visual for conditions shockwave is indicated for: (1)
Based on expert consensus data in sports medicine and musculoskeletal care, shockwave therapy is strongly recommended for a wide range of chronic tendon, bone stress, and select soft-tissue conditions, with agreement rates consistently exceeding 85–100% across expert panels.
The most substantial support exists for chronic tendinopathies, including plantar fasciopathy, insertional and midportion Achilles tendinopathy, patellar tendinopathy, common extensor and medial epicondylopathy, proximal and distal hamstring tendinopathy, and gluteus medius/minimus tendinopathy, where consensus endorsement approaches or reaches 100%.
Shockwave therapy is also supported for calcific rotator cuff tendinopathy, greater trochanteric pain syndrome, and low-grade partial tendon tears, particularly when symptoms are persistent and conservative care alone has failed.
Additionally, there is strong consensus supporting its use in bone-related pathology, including delayed union fractures, non-union fractures, bone stress injuries, and medial tibial stress syndrome, especially in cases lasting longer than three months.
Across these conditions, shockwave therapy is viewed not as a standalone cure, but as an effective adjunct within a multimodal treatment strategy, reinforcing its role as a high-value intervention when applied to the right condition, at the right stage of healing, and in combination with appropriate rehabilitation and load management. Shockwave therapy is a powerful adjunct, but its effectiveness is amplified when combined with manual therapy, exercise, and thoughtful activity modification. Just as we emphasize throughout ChiroUp, clinical success is rarely about one “best” treatment, but about identifying the right recipe of interventions tailored to each unique patient presentation.
-
1. Rhim H.C., et al. (2025). Recommendations for use of extracorporeal shockwave therapy in sports medicine: an international modified Delphi study. British Journal of Sports Medicine, 59(18), 1287-1301.
2. Huang W, Liu Y, Huang C, et al. Extracorporeal shockwave therapy promotes longitudinal bone growth through epiphyseal plate stimulation in adolescent rats. Sci Rep. 2025;15:10234.
3. Lohrer H, Nauck T, Dorn-Lange NV, et al. Extracorporeal shock wave therapy for recalcitrant Osgood-Schlatter disease. Int J Sports Med. 2012;33(6):474-480.
4. Shafshak T, Amer MA. Focused extracorporeal shockwave therapy for youth sports-related apophyseal injuries: case series. Journal of orthopaedic surgery and research. 2023 Aug 22;18(1):616.
5. Omodani T, Sakai T, et al. Shockwave therapy for proximal humeral epiphysiolysis in elite adolescent gymnasts. JSES Int. 2024;8(2):320-326.
6. Spinoso, A. , Settineri, R. , McLaren, C. and Nicolson, G. (2023) Treatment of Peripheral Neuropathy: Combination Therapy Using LED Light, Extracorporeal Shockwave Therapy, Platelet Rich Plasma, and an Oral Dietary Supplement. International Journal of Clinical Medicine, 14, 250-259.
7. Yang L, Li X, Li S, Yang J, Meng D. Effect of extracorporeal shock wave therapy on nerve conduction: a systematic review and meta-analysis. Front Neurol. 2024;15:Article ID 1298456. doi:10.3389/fneur.2024.1298456.
8. Ruiz-Muñoz M, Rueda-Zapata L, Martinez-Barrios F-J, Nováková T, Lopezosa-Reca E, Gonzalez-Sanchez M, Fernandez-Torres R, Galan-Mercant A. Efficacy of Extracorporeal Shockwave Therapy in the Management of Chronic Diabetic Foot Ulcer: A Systematic Review and Meta-Analysis. Medical Sciences. 2025; 13(4):219.