4 Frequently Missed Shoulder Pain Diagnoses
Reading time: 6 minutes
When a patient presents with shoulder pain beginning near their acromion and radiating toward the deltoid tubercle, you probably beam with confidence knowing this has instantly limited your differential diagnosis to…. only about 200 possibilities! 🤷🏼♀️ Yes, unfortunately almost every shoulder complaint shares a similar symptom pattern.
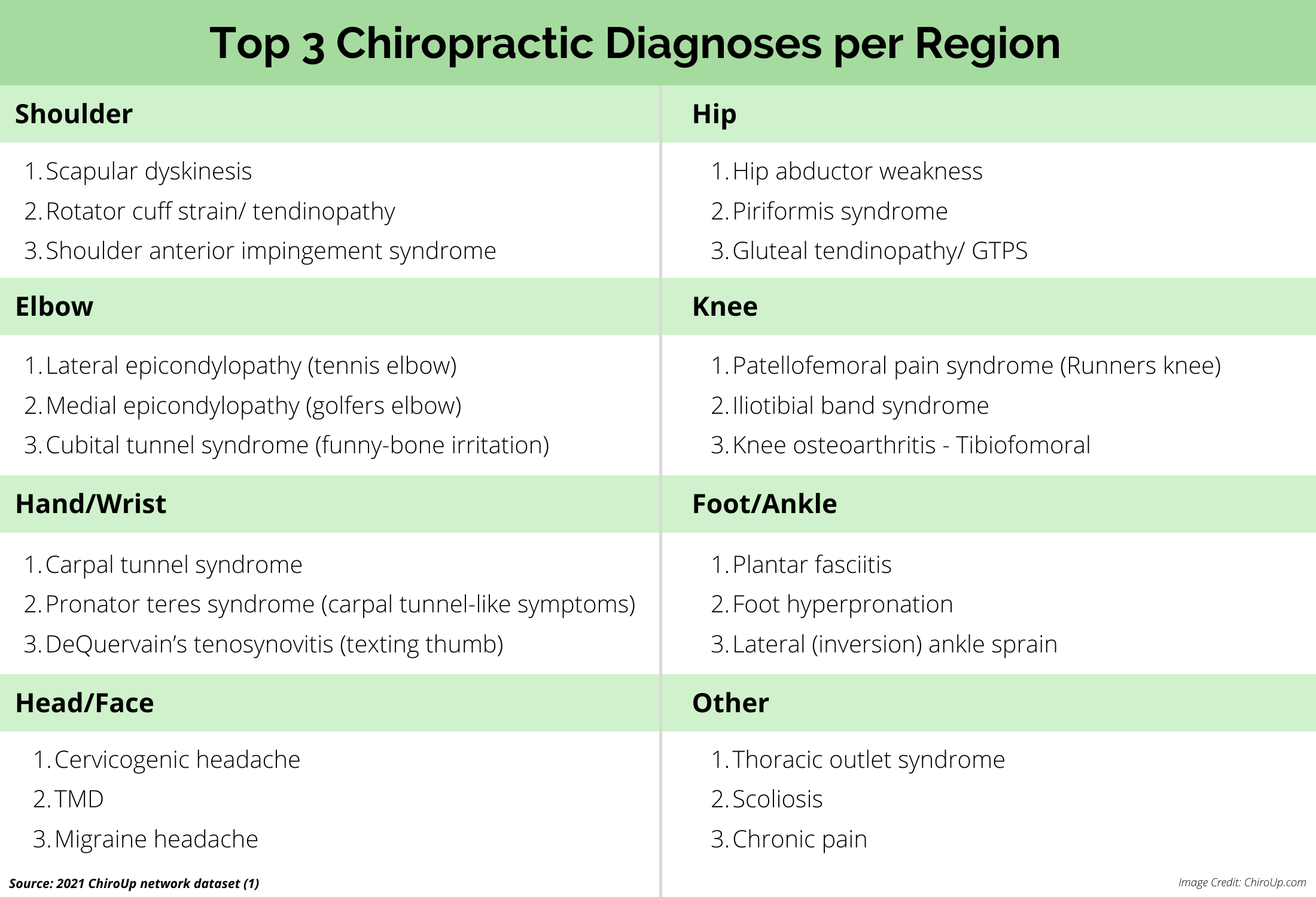
Statistically, the supraspinatus (or one of its close relatives) is the most likely culprit since rotator cuff disorders are the underlying issue in 65% to 70% of patients with shoulder pain. (1-3)
And the recent ChiroUp Clinical Outcomes & Patient Satisfaction Synopsis of over 600,000 unique patient presentations confirm that rotator cuff-related diagnoses occupy the top three shoulder presentations. (4)
But this means something other than the rotator cuff is responsible for the remainder of shoulder pain cases. And unfortunately, many of these rotator-cuff mimicking diagnoses are overlooked - leading to frustration and disappointment for you and your patient.
Fortunately, these rotator cuff look-a-likes often demonstrate valuable clinical clues to help us nail the diagnosis. Here's a quick synopsis of four of the most commonly missed shoulder pain diagnoses and how to tell the difference from rotator cuff pathology.
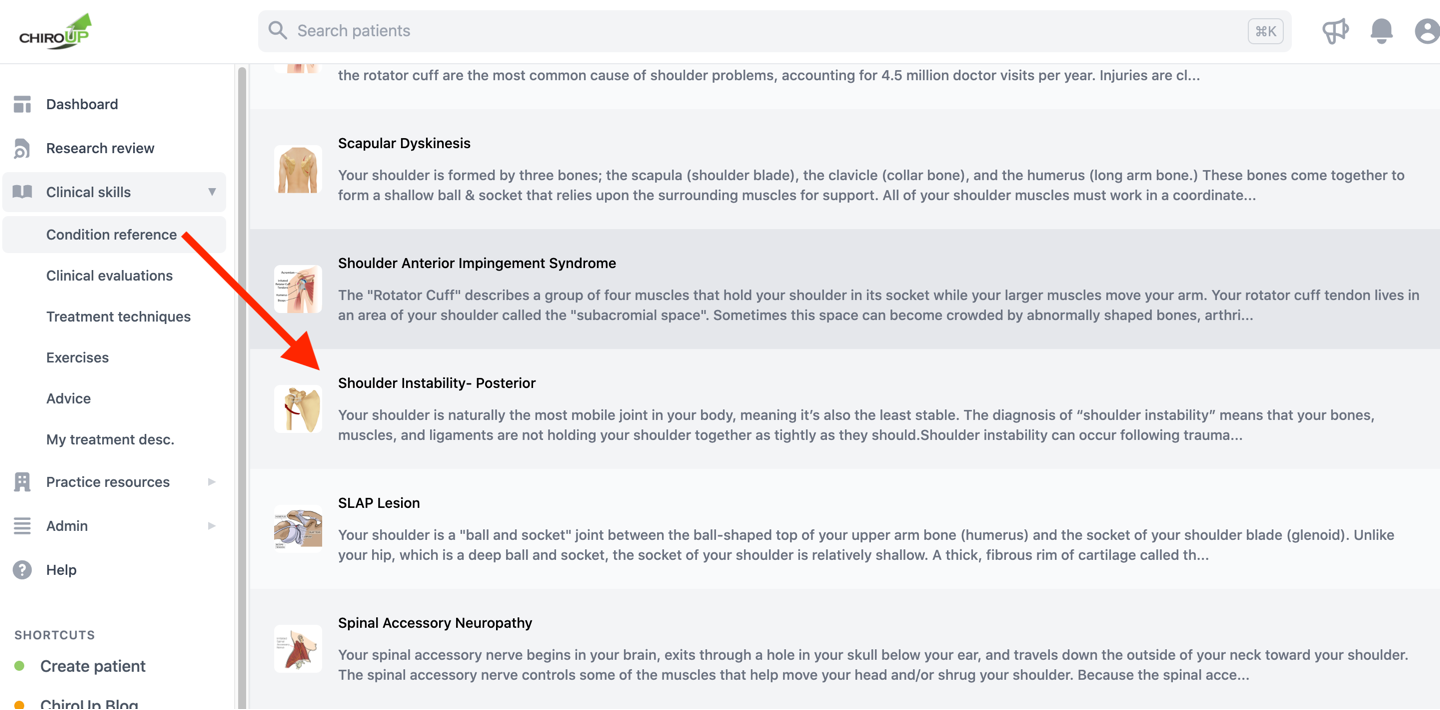
1. Shoulder Instability
Etiology: Acute trauma, or repetitive microtrauma from posture and muscle imbalance, leading to episodic activity-related instability, pain, and loss of function. (5)
How to tell the difference: Instability assessments, including the Load & Shift Test (6,7)
The clinician stabilizes the patient’s shoulder by firmly grasping their trapezius, then uses their opposite hand to grasp the patient’s humeral head while applying a posterolateral, then anteromedial shearing force. Movement greater than 50% of the humeral head width in either direction indicates glenohumeral laxity, i.e., anterior or posterior shoulder instability.
Management: Rehab via shoulder stability exercises (8)
💡 Pro Tip: ChiroUp subscribers can review the new Shoulder Instability protocol for all of the up-to-date best-practice management tutorials for this and 108 other diagnoses. (And if you’re not yet in the club, you can get access in less than a minute by clicking here.)
2. Suprascapular Neuropathy
Etiology: Compression or traction ischemia of the suprascapular nerve as it traverses the suprascapular notch or spinoglenoid notch resulting in shoulder pain or weakness, particularly during cross-body adduction. (9,10)
How to tell the difference: tenderness to palpation over the suprascapular notch and possible weakness or atrophy of the infraspinatus (external rotation). (11,12)
Management:
Myofascial release of the supraspinatus and infraspinatus
Modalities
Avoidance of excessive scapular protraction, cross-body adduction, and overhead movements. (13)
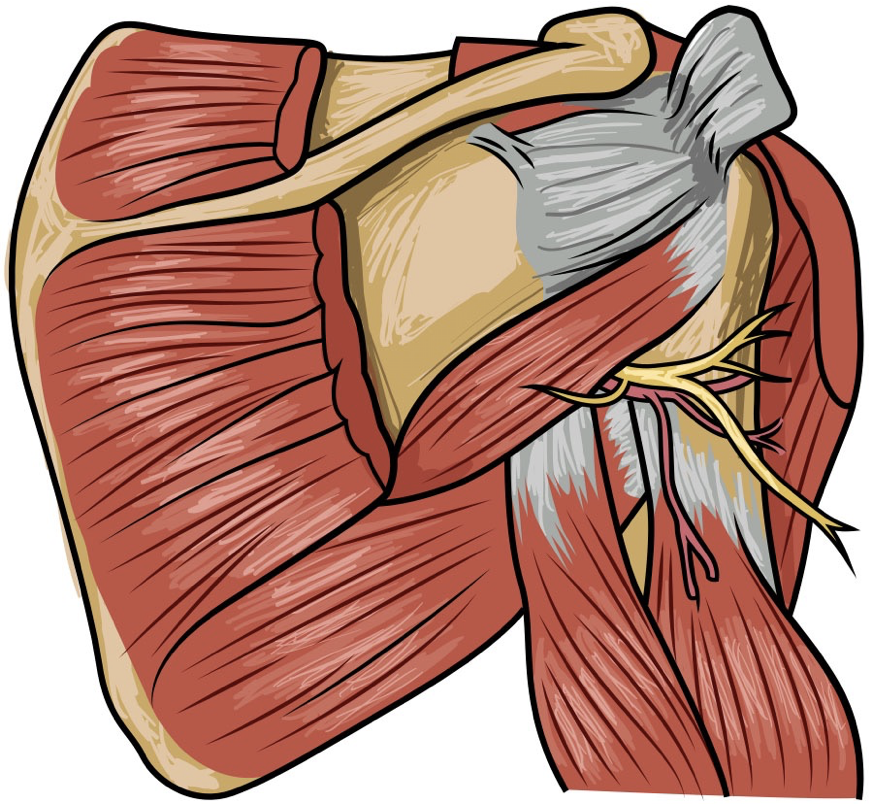
3. Quadrangular Space Syndrome
Etiology: Compression or traction ischemia of the axillary nerve resulting in dull, poorly localized shoulder aching with possible vague deltoid numbness or paresthesia. Also called axillary neuropathy.
How to tell the difference: Symptoms may be exacerbated by placing the arm in a late cocking position while resisting internal rotation. (14,15) Possible weakness or atrophy of the deltoid (abduction) or teres minor (external rotation). Point tenderness at the quadrangular space (QSS sign).
Management:
Selective rest and activity modification, particularly alteration of throwing mechanics and avoiding heavy backpacks (compression) (16-18)
Cross friction massage or myofascial release techniques to the muscles of the quadrangular space teres minor, teres major, and triceps
Cross-body and posterior capsule/ internal rotation stretching
Rotator cuff strengthening (16,19)
Avoid positions that place the axillary nerve in a state of sustained traction (i.e., late cocking)
4. Cervical Referral
AKA: Have you ever focused so intently on catching a non-spinal diagnosis that you overlooked the more obvious possibility?
Etiology: Radiculopathy or scleratogenous referral from irritated cervical nerves, facets, discs, or other soft tissues.
The 2020 EXPOSS study confirmed that many extremity complaints arise from an asymptomatic spine, including up to almost half of all shoulder pain. (20)
This follows earlier research showing that “35% of the patients with shoulder anterior impingement syndrome had cervical nerve root compression on the same side.” (21)
How to tell the difference:
Radiculopathy can be identified via the Spurling test, cervical distraction, upper-Limb tension tests, and limited ipsilateral cervical rotation (<60 degrees). (22)
The arm squeeze test is another valuable means to identify cervical nerve root irritation, with a positive result “in 96.7 % of patients with cervical nerve root compression, compared to 3.87 % of those with rotator cuff [pathology]” (23)
The clinician squeezes the middle third of the upper arm with enough force to create moderate compression of the underlying muscle. Reproduction of arm pain during compression (rated at least VAS 3 on a 0-10 scale) suggests a cervical origin. The rationale is that compression provokes a response from the relatively superficial peripheral nerves (musculocutaneous, radial, ulnar and median) that arise from hypersensitized lower cervical nerve roots (C5-T1).
Management:
Do your thing! Even American Family Physician agrees: “In patients with cervical radiculopathy, exercises and manipulation should focus on stretching and strengthening after the acute pain has subsided.”
Then don’t forget to educate your patients who need to understand why your treatment and their home care are focused on their neck and not solely on their site of pain.
Looking to learn even more about how to deliver the best possible care to your patient suffering from shoulder pain? Check out our webinar: When It’s Not the Rotator Cuff. You’ll leave this webinar with new skills and greater confidence to resolve shoulder complaints, regardless of the diagnosis.
-
1. Jain NB, Fan R, Higgins LD, Kuhn JE, Ayers GD. Does my patient with shoulder pain have a rotator cuff tear? A predictive model from the ROW cohort. Orthopaedic Journal of Sports Medicine. 2018 Jul 16;6(7):2325967118784897. Link
2. Chard M, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology. 1991 Jun;34(6):766-9. Link
3. Vecchio P, Kavanagh R, Hazleman BL, King RH. Shoulder pain in a community-based rheumatology clinic. Rheumatology. 1995 May 1;34(5):440-2. Link
4. Bertelsman TJ, Steele BC, Gower JG. 2021 ChiroUp Network Dataset: Statistical Reporting of 631,970 Clinical Diagnoses Collected from 2212 Evidence-Based Chiropractic Providers Between July 2019- June 2021. Accessed on 07/30/2021 from Link
5. Jaggi A, Lambert S. Rehabilitation for shoulder instability. British journal of sports medicine. 2010 Apr 1;44(5):333-40. Link
6. Mora MV, Ibán MÁ, Heredia JD, Gutiérrez-Gómez JC, Diaz RR, Aramberri M, Cobiella C. Suppl-6, M12: Physical Exam and Evaluation of the Unstable Shoulder. The Open Orthopaedics Journal. 2017;11:946. Link
7. Rockwood CA, editor. The shoulder. Elsevier Health Sciences; 2009.
8. Bateman M, Smith BE, Osborne SE, Wilkes SR. Physiotherapy treatment for atraumatic recurrent shoulder instability: early results of a specific exercise protocol using pathology-specific outcome measures. Shoulder & elbow. 2015 Oct;7(4):282-8. Link
9. Shi LL, Freehill MT, Yannopoulos P, Warner JJ. Suprascapular nerve: is it important in cuff pathology?. Advances in orthopedics. 2012;2012. Link
10. Moen TC, Babatunde OM, Hsu SH, Ahmad CS, Levine WN. Suprascapular neuropathy: what does the literature show?. Journal of shoulder and elbow surgery. 2012 Jun 1;21(6):835-46. Link
11. Ferretti A, De Carli A, Fontana M. Injury of the suprascapular nerve at the spinoglenoid notch. The American journal of sports medicine. 1998 Nov;26(6):759-63. Link
12. Boykin RE, Friedman DJ, Higgins LD, Warner JJ. Suprascapular neuropathy. J Bone Joint Surg Am. 2010 Oct 6. 92(13):2348-64.
13. Skurja Jr M, Monlux JH. Case studies: the suprascapular nerve and shoulder dysfunction. Journal of Orthopaedic & Sports Physical Therapy. 1985 Feb;6(4):254-8. Link
14. Lee S, Saetia K, Saha S, Kline DG, Kim DH. Axillary nerve injury associated with sports. Neurosurgical focus. 2011 Nov 1;31(5):E10.
15. Redler MR, Ruland III LJ, McCue III FC. Quadrilateral space syndrome in a throwing athlete. The American journal of sports medicine. 1986 Nov;14(6):511-3. Link
16. Hoskins WT, Pollard HP, McDonald AJ. Quadrilateral space syndrome: a case study and review of the literature. British journal of sports medicine. 2005 Feb 1;39(2):e9-. Link
17. Cormier PJ, Matalon TA, Wolin PM. Quadrilateral space syndrome: a rare cause of shoulder pain. Radiology. 1988 Jun;167(3):797-8. Link
18. Duralde XA. Neurologic injuries in the athlete's shoulder. Journal of athletic training. 2000 Jul;35(3):316. Link
19. Hammer WI. Functional soft tissue examination and treatment by manual methods: the extremities. Aspen publishers; 1990.
20. Rosedale R, Rastogi R, Kidd J, Lynch G, Supp G, Robbins SM. A study exploring the prevalence of Extremity Pain of Spinal Source (EXPOSS). Journal of Manual & Manipulative Therapy. 2020 Aug 7;28(4):222-30. Link
21. Dernek B, Aydomu S, Duymu TM, Adyeke L, Yardm MY, Kesikta FN, Sindel D, Ketenci A. The incidence of impingement syndrome in cases of cervical radiculopathy: An analysis of 220 cases. Journal of Back and Musculoskeletal Rehabilitation. 2019 Nov 29(Preprint):1-4. Link
22. Eubanks JD. Cervical radiculopathy: nonoperative management of neck pain and radicular symptoms. American family physician. 2010 Jan 1;81(1):33-40. Link
23. Gumina S, Carbone S, Albino P, Gurzi M, Postacchini F. Arm Squeeze Test: a new clinical test to distinguish neck from shoulder pain. European Spine Journal. 2013 Jul;22(7):1558-63. Link