What You Need to Know About TOS
Thoracic outlet syndrome (TOS) is a common diagnosis for evidence-based chiropractors. The condition is characterized by upper extremity pain and paresthesia secondary to occlusion, compression, injury, or irritation to the neurovascular structures traversing the thoracic outlet.
The majority of TOS cases are relatively benign and will respond favorably to conservative care, however, approximately 5% of TOS presentations arise from more threatening origins. This video blog will give you tools to spot ominous presentations and review current best practice evaluations for the remainder.
Neurogenic TOS
Arterial TOS
Venous TOS
Let’s break it down:
Arterial TOS (A-TOS) (blood can’t get in)
Arterial pathology, including (A-TOS) is a vascular problem, but may be due to repetitive mechanical trauma and (is sometimes) misdiagnosed as musculoskeletal injury. (1)
Arterial occlusion of the subclavian artery may occur secondary to stenosis, aneurysm, embolus, or compression from a cervical rib or anomalous first rib. It is the most threatening cause of TOS, accounting for less than 1% of all cases. Signs and symptoms include:
Non-radicular pain of the upper extremity
Pain rarely involves the shoulder or neck
Pain may be present at rest but worsened by elevating the arms above the head.
Possible Raynaud’s phenomenon
Signs of vascular claudication (5 P’s: pain, paralysis, pallor, paresthesia, & pulselessness)
Management:
Urgently refer for emergency management if you suspect A-TOS.
Venous TOS (V-TOS)(blood gets in, but can’t get out)
Subclavian vein obstruction (V-TOS) is the causative mechanism for less than 5% of all cases of TOS. Findings include:
“Deep” pain in the upper extremity, chest, and/or shoulder
Constant symptoms that worsen with activity
Swelling and cyanotic discoloration of the upper extremity
Management:
Refer to emergency management if you suspect V-TOS.
Neurogenic TOS (N-TOS)(irritation to the brachial plexus)
Neurogenic TOS is the most common cause of TOS, accounting for over 95% of all cases. N-TOS results from compression or irritation to the lower trunk or medial cord of the brachial plexus. Symptoms typically include:
Pain, paresthesia, and possible motor weakness in the affected arm
Symptoms are aggravated by elevation of the arms or excessive head and neck movement
Symptoms predominately involve the C8/T1 segmental level and follow an ulnar nerve distribution in 90% of cases
There are three potential sites of compression for N-TOS:
“Scalene” induced TOS occurs from the compression of the neurovascular bundle between the anterior and middle scalene muscles
“Pectoral” compression occurs beneath the pectoralis minor tendon “Costoclavicular” compression happens between the first rib and clavicle
The current evidence-based clinical evaluation of TOS includes (2):
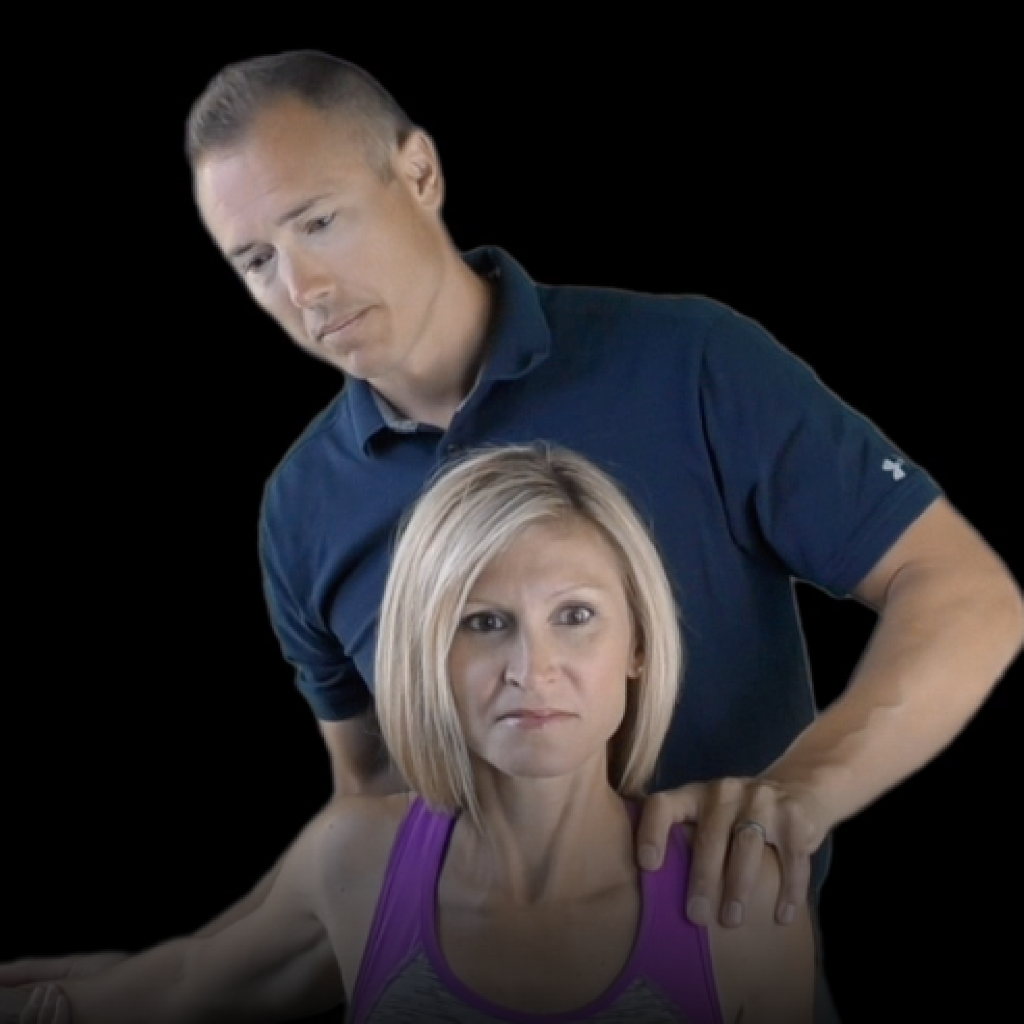
Brachial Plexus Compression Test
This test is positive when deeper palpation of the supraclavicular fossa elicits distal symptoms. Positive in up to 68% of TOS patients. aka Morley test
The clinician stands behind the seated patient and grasps beneath both forearms, holding the elbows at 80 degrees of flexion with the forearms and wrists neutral. The clinician leans the patient’s trunk posteriorly then passively elevates their shoulder girdles. This position is held for up to 3 minutes. A positive result includes either symptom reproduction or paresthesia secondary to a neurovascular release phenomenon.
The clinician monitors the patient’s radial pulse while the seated patient’s arm is taken into in hyperabduction and external rotation. A positive test results in diminution of pulse intensity and reproduction of distal symptoms. Reproduction of TOS complaints implicates pectoral involvement. aka stress hyperabduction test.
The clinician monitors radial pulse while the patient is seated with shoulder in extension, chest in exaggerated military posture. This maneuver is believed to compress the costoclavicular space. A positive test results in diminution of pulse intensity and reproduction of distal symptoms.
Management:
Evidence-based chiropractors provide care to effectively treat N-TOS. A combination of postural advice, manipulation, mobilization, soft tissue therapy, and at-home rehabilitation is the best recipe for these cases.
TOS Clinical Pearls
Weakness, coldness, fatigability, and diffuse arm pain may be arterial TOS and should be referred out (<1%)
Repetitive arm abduction creating edema, cyanosis, and venous dilation may be a sign of venous TOS (<5%)
Symptoms follow an ulnar distribution 90% of the time
TOS is more common in women with some estimates as high as 9:1
Clinicians should assess for potential double crush partners. i.e. cubital tunnel, carpal tunnel, etc.
Up to 23% of cervical soft tissue injuries (whiplash) may include a TOS component
Wouldn’t it be awesome if there were an online library that held all of these best practices for TOS and other common conditions?
Well, guess what… There is.
ChiroUp gives you access to evaluation & rehab for 100+ conditions in a matter of seconds.
This means no more time spent researching and determining what test is the best because we do that part for you – it’s your job to apply them.
Do yourself a favor & get started with an account today.
(We’ll do you a favor & give you your first 14 days for free 🙂)
-
Menon D, Onida S, Davies AH. Overview of arterial pathology related to repetitive trauma in athletes. J Vasc Surg. 2019 May 18. pii: S0741-5214(19)30202-2.
Horris HB et al. The Diagnostic Accuracy of Clinical Diagnostic Tests for Thoracic Outlet Syndrome. Journal of Sport Rehabilitation, 2017, vol. 26, issue 5, p 459