What is the most common cause of hip pain?
Reading time: 7 minutes
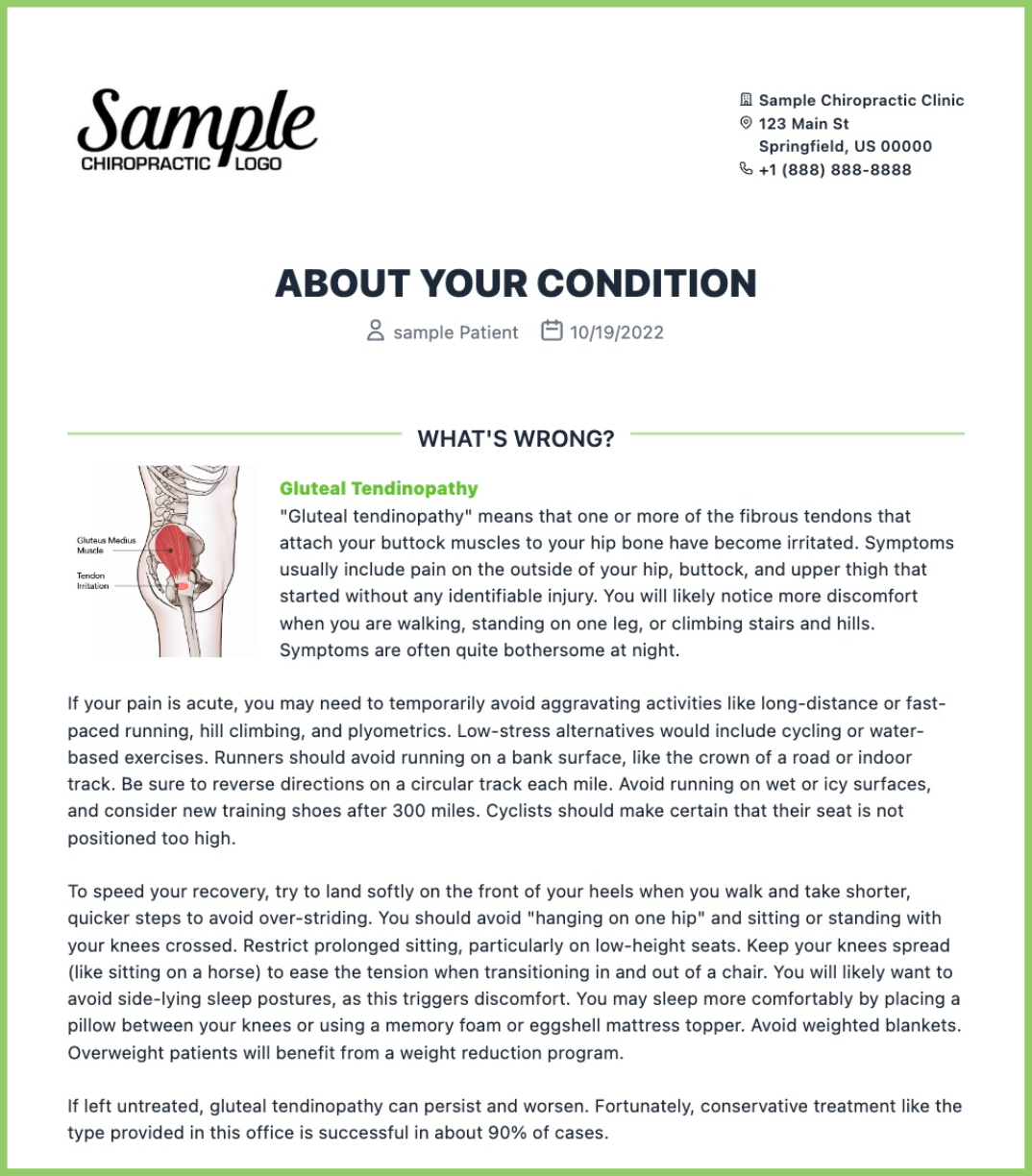
Tendinopathy involving the gluteus medius or gluteus minimus is the most common cause of lateral hip pain. (1, 2) Gluteal tendon tears have been dubbed "rotator cuff tears of the hip" because of their similar prevalence, anatomy, etiology, and management.
Lateral hip pain is rarely an inflammatory problem.
While the greater trochanteric bursa was once a focal point for lateral hip pain, current thought deemphasizes the concept of "bursitis." Evidence now suggests that true "bursitis" is rare and, if present, generally occurs secondary to another underlying dysfunction, like gluteal tendinopathy. (3, 4) Only 10-20% of patients with lateral hip pain exhibit bursal enlargement. (2, 5) Even when the bursa is involved, histologic studies fail to show signs of inflammation. (6)
Chiropractic treatment is only effective if we can identify the cause of pain. Injecting painful tissue with a corticosteroid would provide only temporary relief and not address the etiology of tissue degeneration. However, recently PRP injections have shown promise in helping chronic cases recover quickly. (7)
What causes Gluteal Tendinopathy?
Gluteal tendinopathy (GT) develops from excessive tension or compression. Similar to rotator cuff tendinopathy, the primary trigger for gluteus medius tendinopathy seems to be compression of the undersurface of the tendon. (8) Hypothetically, if an excessive tensile load were the primary mechanical trigger, tears of the outermost fibers would predominate. While the deeper fibers carry the least tensile load, they experience the highest compressive loads at their bony insertion. (8) Long-term compressive loads lead to a predictable continuum of ischemia, failed healing, matrix degradation, diminished load-bearing capacity, and failure. (8, 9)
What are the signs and symptoms of Gluteal Tendinopathy?
Lateral hip pain
Exacerbated during side lying on the affected side
Increased pain while ascending or descending stairs and during long periods of standing
Tenderness to palpation over the greater trochanter
Nighttime pain (9)
How can YOU test for Gluteal Tendinopathy?
Magnetic resonance imaging is the gold standard for this investigation. However, some orthopedic tests are easy to perform and demonstrate high sensitivity and specificity for GT.
Hip Lag Sign
Begin with the patient in a side-lying position, affected side up. The clinician stabilizes the patient’s pelvis with one hand while using the other to passively move the patient’s hip and thigh into 20 degrees of abduction, 10 degrees of extension, and maximal internal rotation. The patient’s leg should remain relaxed with the knee bent at 45 degrees. After asking the patent to hold their leg in this position actively, the clinician releases support. The test is positive if the patient is unable to maintain this position and their foot drops more than 10 cm. (10)
The Hip Lag Sign demonstrates high sensitivity (89.5%) and specificity (96.6%) for detecting hip abductor tendon injury. (Glut Max, Glute Med and TFL) (10)
FABREX Test
Begin with a patient supine with legs in full extension. The clinician begins by holding the affected side ankle with their distal hand and supporting the ipsilateral knee with the superior hand. Then, passively move the patient's affected limb into 90° hip and knee flexion. Once the hip and knee are in 90°of flexion, passively abduct the hip to 50°. Finally, while continually stabilizing the knee, slowly perform passive external rotation to assess for the reproduction of lateral hip pain.
The FABREX test, when positive, can be used to determine the diagnosis of gluteal tendinopathies with high specificity. Moreover, it has high sensitivity, excluding the diagnosis when negative. (11)
What is the difference Between FABER Test and FABREX Test
When is it not Gluteal Tendinopathy?
Presence of leg numbness or pain radiating significantly beyond the knee. (12)
Patients with lateral hip pain with no palpable tenderness over the greater trochanter. (13)
Check out this recent blog reviewing a similar test identifying other hip diagnoses.
What are your treatment options for Gluteal Tendinopathy?
GT treatment goals include:
1. Eliminating modifiable risk factors and faulty mechanics that cause excessive tensile or compressive loading.
2. Implementing early and progressive restorative loading to improve tendon integrity and load-bearing capacity. (14)
Next time you encounter a patient with lateral hip pain, use these two orthopedic tests. Treatment becomes easy once you have the correct diagnosis. Check out the most evidence-based practical exercises and treatment strategies in the condition reference section of ChiroUp.
-
1. Bancroft LW, Blankenbaker DG. Imaging of the tendons about the pelvis. American Journal of Roentgenology. 2010 Sep;195(3):605-17. Link
2. Long SS, Surrey DE, Nazarian LN. Sonography of greater trochanteric pain syndrome and the rarity of primary bursitis. American Journal of Roentgenology. 2013 Nov;201(5):1083-6. Link
3. Pfirrmann CW, Notzli HP, Dora C, Hodler J, Zanetti M. Abductor tendons and muscles assessed at MR imaging after total hip arthroplasty in asymptomatic and symptomatic patients. Radiology. 2005 Jun;235(3):969-76. Link
4. Woodley SJ, Nicholson HD, Livingstone V, Doyle TC, Meikle GR, Macintosh JE, Mercer SR. Lateral hip pain: findings from magnetic resonance imaging and clinical examination. journal of orthopaedic & sports physical therapy. 2008 Jun;38(6):313-28. Link
5. Connell DA, Bass C, Sykes CJ, Young D, Edwards E. Sonographic evaluation of gluteus medius and minimus tendinopathy. European radiology. 2003 Jun 1;13(6):1339-47. Link
6. Silva F, Adams T, Feinstein J, Arroyo RA. Trochanteric bursitis: refuting the myth of inflammation. JCR: Journal of Clinical Rheumatology. 2008 Apr 1;14(2):82-6. Link
7. Fitzpatrick J, Bulsara MK, O’Donnell J, McCrory PR, Zheng MH. The effectiveness of platelet-rich plasma injections in gluteal tendinopathy: a randomized, double-blind controlled trial comparing a single platelet-rich plasma injection with a single corticosteroid injection. The American journal of sports medicine. 2018 Mar;46(4):933-9.
8. Almekinders LC, Weinhold PS, Maffulli N. Compression etiology in tendinopathy. Clinics in sports medicine. 2003 Oct 1;22(4):703-10. Link
9. Grimaldi A, Fearon A. Gluteal tendinopathy: integrating pathomechanics and clinical features in its management. Journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):910-22. Link
10. Kaltenborn A, Bourg CM, Gutzeit A, Kalberer F. The Hip Lag Sign-prospective blinded trial of a new clinical sign to predict hip abductor damage. PLoS one. 2014 Mar 12;9(3):e91560. Link
11. Freitas A, Rosa TM, MACEDO NETO SL, Bandeira VD, SOUTO DR, Barin FR. FABREX: A NEW CLINICAL TEST FOR DIAGNOSIS GLUTEAL TENDINOPATHY. Acta Ortopédica Brasileira. 2022 Apr 15;30. Link
12. Jennings F, Lambert E, Fredericson M. Rheumatic diseases presenting as sports-related injuries. Sports Medicine. 2008 Nov 1;38(11):917-30. Link
13. Grimaldi A, Mellor R, Nicolson P, Hodges P, Bennell K, Vicenzino B. Utility of clinical tests to diagnose MRI-confirmed gluteal tendinopathy in patients presenting with lateral hip pain. British journal of sports medicine. 2017 Mar 1;51(6):519-24. Link
14. Cook JL, Purdam CR. The challenge of managing tendinopathy in competing athletes. Br J Sports Med. 2014 Apr 1;48(7):506-9. Link