Maigne Syndrome: The #1 Overlooked LBP Diagnosis?
Maigne syndrome and cluneal neuropathy are commonly overlooked causes of pain in the lumbosacral region, iliac crest, and buttock. (1-3) In fact, the pair are causative or contributory in up to 40% of LBP cases. (5,40,41) And that prospect increases as symptoms extend over the posterior iliac crest. (2)
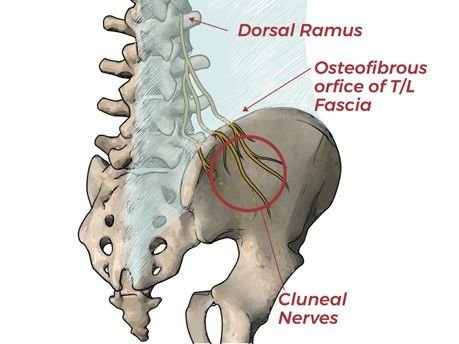
Maigne syndrome typically results from irritation of a thoracolumbar dorsal ramus. (3) Facet joint dysfunction, degeneration, and instability are common culprits. Maigne syndrome is particularly elusive because the anatomical site of origin is often asymptomatic. (3)This blog will cover the essentials of management, including a 5-minute video tutorial detailing the top assessments, treatments, and exercises, plus our top 10 clinical pearls.
Maigne syndrome/ Cluneal neuropathy is the newest ChiroUp protocol, and we’re particularly excited because it’s the 100th ChiroUp protocol.
How are ChiroUp Protocols Developed?
Our research team scours several online databases for the latest evidence-based data regarding a condition’s etiology and clinical presentation, plus the most appropriate assessment, imaging/tests, differential diagnosis, treatment, exercises, and ADL’s.
Our writers summarize that data into a condition protocol draft.
The draft is submitted to our board of advisors and invited expert guests for a 14-day comment & critique period.
The protocol is updated to reflect the peer-review recommendations, then published to our website after final approval.
The protocol is continually refined as new data emerges, and by surveying our top performers for their real-world advice.
Subscribers can visit the ChiroUp condition reference library to access the entire synopsis, but here are our top 10 clinical pearls for Maigne syndrome and cluneal neuropathy:
2. Distal entrapments of the cluneal nerve are thought to increase neurodynamic tension on the dorsal nerve root, thereby compounding ischemia and hyperexcitability. (7,8) Maigne syndrome and superior cluneal nerve entrapment frequently coexist as double crush partners.
3. The most common manifestation of Maigne syndrome is low back pain that mirrors the presentation of lumbosacral or sacroiliac joint dysfunction. (3,9) Complaints rarely affect the thoracolumbar junction itself. (3)
4. Symptoms of a peripheral cluneal nerve entrapment frequently mimic those of lumbar stenosis - in that both conditions are provoked by prolonged standing or walking. (8)
5. In cases of peripheral cluneal nerve entrapment, patients will often report palpatory tenderness at the primary site of entrapment on the posterior iliac crest, approximately 3–4 cm (medial branch) or 7–8 cm (intermediate/ middle branch) from the midline. (8,12,40)
6. Paradoxical dysfunctional breathing may contribute to thoracolumbar stress. Clinicians should look for classic signs of dysfunctional breathing, including elevation of the upper rib cage, inadequate or asymmetrical lateral rib cage expansion, excessive paraspinal muscle contraction, or initiation of breathing from the chest rather than the abdomen. (29)
7. Gait assessment may reveal contributory mechanics, including diminished or asymmetrical arm swing (loss of glenohumeral motion), loss of hip extension, or short stride length. (45)
8. Motion palpation and clinical assessment may demonstrate signs of thoracolumbar hypomobility or hypermobility; and differentiating between the two is essential. Loss of spinal stability is a common precipitating factor for Maigne syndrome. (18)
9. Specific treatment strategies will be chosen based on whether the primary problem involves hypermobility or hypomobility. Hypermobile joints require a focus on building stability, whereas hypomobile joints, particularly degenerated segments, prefer strategies that open the intravertebral foramen.
10. Stiff fascia reduces muscle contractility and can perpetuate a chronic ischemic compartment-like syndrome. Many providers advocate for using shock wave therapy or mechanical cupping before stretching for multi-dimensional release of the thoracolumbar fascia.
Ready to put this information to work?
Wouldn’t it be great to have all of this information in one concise protocol that you can access 24/7 and use to educate your patients in seconds?
Well, with ChiroUp, you can.
And not only will you have access to our protocol for Maigne Syndrome & Cluneal neuropathy, but you’ll also have access to 100+ other conditions.
For more information on Maigne Syndrome, check out this podcast episode!
-
Maigne JY, Maigne R. Trigger point of the posterior iliac crest: painful iliolumbar ligament insertion or cutaneous dorsal ramus pain? An anatomic study. Archives of physical medicine and rehabilitation. 1991 Sep 1;72(10):734-7. Link
Kim SR, Lee MJ, Lee SJ, Suh YS, Kim DH, Hong JH. Thoracolumbar junction syndrome causing pain around posterior iliac crest: a case report. Korean journal of family medicine. 2013 Mar;34(2):152. Link
Cain L. Maigne’s Syndrome. HFE Health and Fitness Education. 2020 Jan 14. Link
Proctor D, Dupuis P, Cassidy JD. Thoracolumbar syndrome as a cause of low-back pain: a report of two cases. The Journal of the Canadian Chiropractic Association. 1985 Jun;29(2):71. Link
Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K, Hokari M, Isobe M, Kusano M. Association between intermittent low-back pain and superior cluneal nerve entrapment neuropathy. Journal of Neurosurgery: Spine. 2016 Feb 1;24(2):263-7. Link
Pećina MM, Krmpotić-Nemanić J, Markiewitz AD. Tunnel Syndromes: Peripheral Nerve Compression Syndromes. Boca Raton, FL: CRC Press LLC; 2001.
Noh K, Jung JB, Seong JW, Kim DE, Kwon D, Kim Y. Thoracolumbar Junction Syndrome Accompanying Renal Artery Stenosis: A Case Report. Annals of Rehabilitation Medicine. 2020 Feb 29;44(1):85-9. Link
Chiba Y, Isu T, Kim K, Iwamoto N, Morimoto D, Yamazaki K, Hokari M, Isobe M, Kusano M. Association between intermittent low-back pain and superior cluneal nerve entrapment neuropathy. Journal of Neurosurgery: Spine. 2016 Feb 1;24(2):263-7. Link
Maigne R. Low back pain of thoracolumbar origin (T11-T12-L1). Diagnosis and treatment of pain of vertebral origin. 2nd ed. Boca Raton: Tayloe and Francis Group. 2006:289-98.
Noh K, Jung JB, Seong JW, Kim DE, Kwon D, Kim Y. Thoracolumbar Junction Syndrome Accompanying Renal Artery Stenosis: A Case Report. Annals of Rehabilitation Medicine. 2020 Feb 29;44(1):85-9. Link
Aktas İ, Akgün K, Palamar D, Saridogan M. Thoracolumbar junction syndrome: An overlooked diagnosis in an elderly patient. Turkish Journal of Geriatrics/Türk Geriatri Dergisi. 2014 Apr 1;17(2). Link
Flynn T, Fritz J, Whitman J, Wainner R, Magel J, Rendeiro D, Butler B, Garber M, Allison S. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002 Dec 15;27(24):2835-43. Link
Aoun F, Malek E, Kazan D, Albisinni S, Peltier A, Bollens R, Roumeguère T. Management of chronic testicular pain due to thoracolumbar junction syndrome: A pilot study. Progrès en Urologie. 2020 Jan 21. Link
Alptekin K, Örnek NI, Aydın T, Alkan M, Toprak M, Balcı LA, Alptekin JÖ. Effectiveness of exercise and local steroid injections for the thoracolumbar junction syndrome (the Maigne’s syndrome) treatment. The open orthopaedics journal. 2017;11:467. Link
Zhou L., Schneck C.D., Shao Z. The anatomy of dorsal ramus nerves and its implications in lower back pain. Neurosci. Med.2012;3:192–201. doi: 10.4236/nm.2012.32025.
DiMond ME. Rehabilitative principles in the management of thoracolumbar syndrome: a case report. Journal of chiropractic medicine. 2017 Dec 1;16(4):331-9. Link
Frisch H.Programmierte Untersuchung Des Bewegungsapparates. Berlin: Springer-Verlag; 1983.
Alptekin K, Örnek NI, Aydın T, Alkan M, Toprak M, Balcı LA, Alptekin JÖ. Effectiveness of exercise and local steroid injections for the thoracolumbar junction syndrome (the Maigne’s syndrome) treatment. The open orthopaedics journal. 2017;11:467. Link
Frank C, Kobesova A, Kolar P. Dynamic neuromuscular stabilization & sports rehabilitation. International journal of sports physical therapy. 2013 Feb;8(1):62. Link
Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Archives of physical medicine and rehabilitation. 2005 Sep 1;86(9):1753-62. Link
Fritz JM, Whitman JM, Childs JD. Lumbar spine segmental mobility assessment: an examination of validity for determining intervention strategies in patients with low back pain. Archives of Physical Medicine and Rehabilitation. 2005 Sep 1;86(9):1745-52. Link
Liebenson C, Karpowicz AM, Brown SH, Howarth SJ, McGill SM. The active straight leg raise test and lumbar spine stability. PM&R. 2009 Jun 1;1(6):530-5. Link
Hicks GE, Fritz JM, Delitto A, Mishock J. Interrater reliability of clinical examination measures for identification of lumbar segmental instability. Archives of physical medicine and rehabilitation. 2003 Dec 1;84(12):1858-64. Link
Nachemson A. Lumbar spine instability. A critical update and symposium summary. Spine. 1985 Apr;10(3):290-1. Link
Ogon M, Bender BR, Hooper DM, Spratt KF, Goel VK, Wilder DG, Pope MH. A dynamic approach to spinal instability: Part I: Sensitization of intersegmental motion profiles to motion direction and load condition by instability. Spine. 1997 Dec 15;22(24):2841-58. Link
Delitto A, Erhard RE, Bowling RW. A treatment-based classification approach to low back syndrome: identifying and staging patients for conservative treatment. Physical therapy. 1995 Jun 1;75(6):470-85. Link
Waddell G, Somerville D, Henderson I, Newton M. Objective clinical evaluation of physical impairment in chronic low back pain. Spine. 1992 Jun;17(6):617-28. Link
Morgan, WE. Cluneal Nerve Entrapment: Lumbo-Pelvic Pain Part 2. Accessed 04/28/20 from: http://drmorgan.info/clinicians-corner/cluneal-nerve-entrapment/
Kolá P, Šulc J, Kyn l M, Šanda J, Akrt O, Andel R, Kumagai K, Kobesová A. Postural function of the diaphragm in persons with and without chronic low back pain. Journal of orthopaedic & sports physical therapy. 2012 Apr;42(4):352-62. Link
Walker HK, Hall WD, Hurst JW. The Oral Cavity and Associated Structures--Clinical Methods: The History, Physical, and Laboratory Examinations. Butterworths; 1990.
Aktas İ, Akgun K. Thoracolomber junction syndrome. Bogazici Tip Dergisi. 2014;1(1):29-31.
Langevin HM, Fox JR, Koptiuch C, Badger GJ, Greenan-Naumann AC, Bouffard NA, Konofagou EE, Lee WN, Triano JJ, Henry SM. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC musculoskeletal disorders. 2011 Dec 1;12(1):203. Link
Seong JW. Principle and insight into pain. Paju, Korea: Koonja Press; 2012. p.844–55.
Branchini M, Lopopolo F, Andreoli E, Loreti I, Marchand AM, Stecco A. Fascial Manipulation® for chronic aspecific low back pain: a single blinded randomized controlled trial. F1000Research. 2015;4. Link
Kim SR, Lee MJ, Lee SJ, Suh YS, Kim DH, Hong JH. Thoracolumbar junction syndrome causing pain around posterior iliac crest: a case report. Korean journal of family medicine. 2013 Mar;34(2):152. Link
Morgan, WE. Maigne's Syndrome: Lumbo-Pelvic Pain Part 1. Accessed 04/28/20 from: http://drmorgan.info/clinicians-corner/maigne-s-syndrome/. Link
Maigne R. Diagnosis and treatment of pain of vertebral origin: a manual medicine approach. Baltimore: Williams & Wilkins; 1996.
Maigne JY, Doursounian L. Entrapment neuropathy of the medial superior cluneal nerve: Nineteen cases surgically treated, with a minimum of 2 years' follow-up. Spine. 1997 May 15;22(10):1156-9. Link
Kuniya H, Aota Y, Kawai T, Kaneko KI, Konno T, Saito T. Prospective study of superior cluneal nerve disorder as a potential cause of low back pain and leg symptoms. Journal of orthopaedic surgery and research. 2014 Dec;9(1):139. Link
Isu T, Kim K, Morimoto D, Iwamoto N. Superior and Middle Cluneal Nerve Entrapment as a Cause of Low Back Pain. Neurospine. 2018;15(1):25‐32. Link
Maigne R. Low back pain of thoracolumbar origin. Archives of physical medicine and rehabilitation. 1980 Sep;61(9):389-95. Link
Cui HS, Hong AR, Kim JB, Yu JH, Cho YS, Joo SY, Seo CH. Extracorporeal shock wave therapy alters the expression of fibrosis-related molecules in fibroblast derived from human hypertrophic scar. International journal of molecular sciences. 2018 Jan;19(1):124. Link
Mulligan BR. Mobilisations with movement (MWM'S). Journal of Manual & Manipulative Therapy. 1993 Jan 1;1(4):154-6. Link
Mulligan BR. Manual Therapy: NAGS, SNAGS, MWM etc. 6th Ed. Plane View Services Ltd. Wellington, NZ. 2010
Tucker J. “Maigne Syndrome” Message to Tim Bertelsman regarding advice on chiropractic management of Maigne syndrome patients via direct email on 05/02/2020.