Maigne Syndrome: Sciatica of the Thoraco-Lumbar Junction
Lateral hip, lumbosacral, and groin pain are often due to lumbar spine or hip joint dysfunction. However, the next time you see these symptoms, be sure to assess the thoracolumbar junction (TLJ). TLJ dysfunction, often described as Maigne Syndrome, may result in nerve irritation with referral to the lumbopelvic region. Proper assessment and treatment results in highly satisfied patients. In the next ten minutes, you will learn five tips about why Maigne syndrome should be on your shortlist of differential diagnoses.
1. What is Maigne Syndrome?
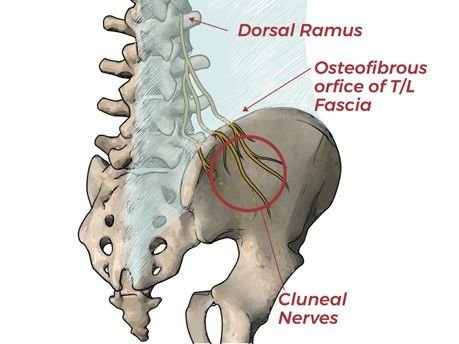
Maigne syndrome is an often-overlooked source of lower back, hip, and groin discomfort. Spinal dysfunction leading to pain and degeneration is common at transitional sites like the TLJ. The sagittally-aligned lumbar facets limit rotation. In contrast, the thoracic spine rotates much more freely due to the frontal plane alignment of its facets. Rotation and sustained flexion impose stress to this area. Irritation often affects the primary posterior ramus of the TLJ, resulting in radiating symptoms, aka Maigne Syndrome. Patients with Maigne Syndrome typically present with primary hip and groin pain, occasionally accompanied by LBP. Symptoms may also refer to the lower abdomen, pubic region, iliac fossa, posterior iliac crest, buttock, and testicle, or labia.
2. Clinical Examination
Upon physical examination, Maigne Syndrome patients present without impairments in the hip, and have normal lower-quarter neurological and neurodynamic tests. Nerve irritation at the TLJ affects the posterior ramus - resulting in radiating pain along the cluneal nerves. Degeneration of the facet joints in and around the thoracolumbar junction may also contribute to nerve irritation.
Maigne Syndrome Clinical Prediction Rule
Adapted from Proctor et al. (1)
“Deep” pain with tenderness to palpation over the iliac crest at the point where the distal cluneal nerve branches across the iliac crest.
Hypersensitivity of the skin and subcutaneous tissues of the gluteal and iliac crest.
Localized tenderness to the PA shear test over the affected thoracolumbar segment, i.e., pressure at the TLJ will reproduce local discomfort and, on occasion, referred pain.
May be associated with ipsilateral sacroiliac joint dysfunction.
Absent nerve root tension signs.
Radiographic findings are commonly unremarkable.
3. Differential Diagnosis of Lumbopelvic Pain
Etiology: Hip
Consider the C-sign. If positive, direct your evaluation to hip orthopedic tests. FABER and FADIR tests can often isolate the femoral acetabular joint as the source of pain.Remember: Isolated hip motion will not illicit symptoms if the TLJ is the primary dysfunction.
Etiology: Lumbar Spine
Upper lumbar disc lesions may also refer to the groin, lateral hip, and lower back. A study by Kido (2) found that lumbar radicular pains are affected by hip movement. Hip flexion tensions the sciatic nerve (L4-S1 levels), while hip extension tensions the femoral nerve (L1-3), Use the Straight Leg Raise and Femoral Nerve Tension test to determine if pain is potentially originating from the lumbar spine. If TLJ dysfunction is the culprit, hip flexion and extension should not affect symptoms.
Etiology: TLJ
Hip, groin, and lower back pain is elicited during moments that exploit rotation and extension of the thoracolumbar junction. Kemps and Sphinx maneuvers are common ways to test the TL junction. Spinal Motion palpation and PA Shear Test can identify irritation of inflammation around the TL junction. Remember, a positive test will reproduce the patient’s symptoms; localized spinal pain at the TLJ is not positive for Maigne Syndrome. Instead, a positive test must reproduce groin, lateral hip, or lower back pain.
4. Management of Maigne Syndrome
Manipulation
Original research by Maigne , and an early case study by Proctor et al., support the use of spinal manipulation to reduce pain and alleviate symptoms of Maigne Syndrome. (1,3)
Neural Desensitization Maneuvers
Neurodynamic techniques release local adhesions of the cluneal nerves at the thoracolumbar aponeurosis. Neural mobilization optimizes the ability of mechanical interfaces to glide relative to the neural structure. Active and passive stretching diminishes intraneural edema and pressure by mobilizing the peripheral nerve as well as associated vascular structures. (4,5)
Injections
The allopathic conservative approach for cluneal nerve entrapment includes an anesthetic nerve block and anti-inflammatory steroid injections. If these treatment approaches are unsuccessful, then surgery. (6)
5. Conclusion
TLJ syndrome commonly presents as unilateral pain in the lower lateral region of the spine, groin pain and/or an aching or painful sensation that radiates above and along the pelvis and into the pubic region. Watch for the full Maigne Syndrome condition reference (protocol # 100 !!!) coming soon to the ChiroUp library.
We’re talking the most up-to-date & evidence-based video demonstrations for every test, treatment, & exercise for Maigne Syndrome in one concise protocol.
How would you like to have access to this protocol? (Think: this blog, but easier to read and at your fingertips.)
Well, guess what? YOU CAN!
And not only that, but with ChiroUp, you can then transfer that information into a report for your patients in a matter of seconds?
Visit ChiroUp.com today to see how to get started - you’re not going to want to miss out on this release!
-
Proctor D, Dupuis P, Cassidy JD. Thoracolumbar syndrome as a cause of low-back pain: a report of two cases. The Journal of the Canadian Chiropractic Association. 1985 Jun;29(2):71. Link
Kido T, Okuyama K, Chiba M, Sasaki H, Seki N, Kamo K, Miyakoshi N, Shimada Y. Clinical diagnosis of upper lumbar disc herniation: Pain and/or numbness distribution are more useful for appropriate level diagnosis. Journal of Orthopaedic Science. 2016 Jul 1;21(4):419-24. Link
Maigne R. Low back pain of thoracolumbar origin. Arch Phys Med Rehabil. 1980;61(9):389-395. Link
Boudier-Revéret M, Gilbert KK, Allégue DR, Moussadyk M, Brismée JM, Sizer Jr PS, Feipel V, Dugailly PM, Sobczak S. Effect of neurodynamic mobilization on fluid dispersion in median nerve at the level of the carpal tunnel: A cadaveric study. Musculoskeletal Science and Practice. 2017 Oct 1;31:45-51. Link
Gilbert KK, Smith MP, Sobczak S, James CR, Sizer PS, Brismée JM. Effects of lower limb neurodynamic mobilization on intraneural fluid dispersion of the fourth lumbar nerve root: an unembalmed cadaveric investigation. Journal of Manual & Manipulative Therapy. 2015 Oct 20;23(5):239-45 Link
Morimoto D, Isu T, Kim K, et al. Long-term outcome of surgical treatment for superior cluneal nerve entrapment neuropathy. Spine (Phila Pa 1976). 2017;42(10):783-788. Link