Chiropractic Treatment for Cuboid Syndrome
Cuboid syndrome is a condition often challenging to identify and frequently misdiagnosed. Chiropractors should consider cuboid syndrome as a potential cause of lateral foot and ankle pain. Conservative treatment, particularly specific cuboid manipulation techniques, yields favorable outcomes, often leading to a decrease or cessation of symptoms post-treatment. Given the limited utility of radiographic imaging, diagnosis primarily relies on patient history and clinical signs and symptoms, emphasizing the importance of understanding the syndrome's underlying causes for accurate diagnosis and treatment.
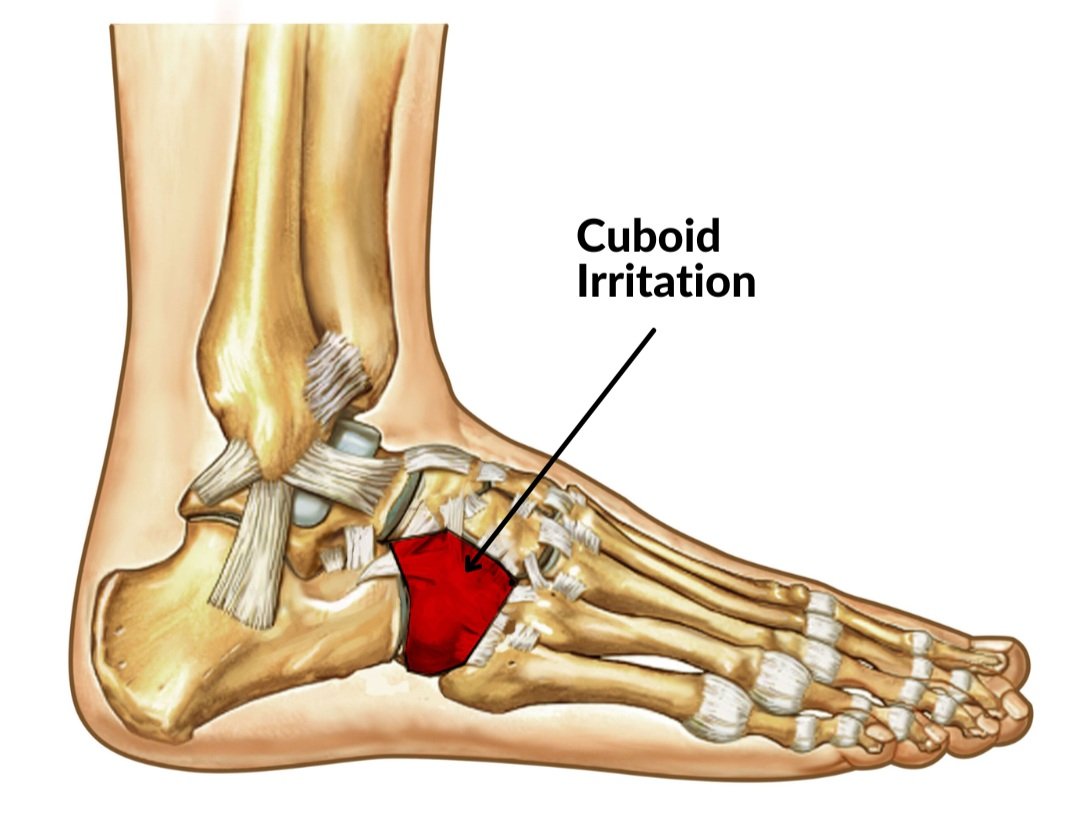
Various populations of people are susceptible to cuboid syndrome. Among athletes with foot injuries, as many as 4% presented with cuboid syndrome. This number increases to 6.7% of patients suffering from co-existent inversion ankle sprains. (1,2) Understanding the foot's anatomy is crucial, particularly for diagnosing cuboid syndrome. Among the 26 bones in the foot, the cuboid stands out as the sole bone that interacts with the tarsometatarsal and midtarsal joints. It connects the lateral column and the transverse plantar arch, providing essential stability to the foot. This unique role makes the cuboid a keystone in maintaining the foot's rigidity and static structure. Joint dysfunction arises from poor balance and foot stability during athletic activity.
Cuboid Syndrome: A Typical Subjective Note
Patients typically present with pain:
Developed rapidly or gradually over time
Resulting from an inversion ankle sprain
Pain is usually located directly over the cuboid
Pain may radiate into:
Plantar medial arch
Distally along the fourth metatarsal
Pain experienced during:
Normal weight-bearing (Sharp)
Non-weight-bearing (Achy)
Weakness during the toe-off of the propulsive phase of the gait cycle
Cuboid Syndrome: A Typical Objective Note
Midtarsal Supination Test
The clinician firmly grasps the patient's heel and forefoot. The clinician applies a shearing force through the mid-tarsal joint via inversion and plantarflexion. Reproduction of pain over the cuboid suggests cuboid syndrome. (2)
*Notice the inclusion of the modified slump test and signs of inflammatory arthropathy. Dural tension orthopedic tests rule out radicular symptoms extending into the foot arch. Check out this infographic, which is commonly used in chiropractic offices to rule out inflammatory arthropathy.
Cuboid Syndrome: A Typical Assessment
Cuboid syndrome persists for one month and may need two to four manipulations. (1,2)
Avoid high-impact activities if your patient is still symptomatic.
Patients may return to vigorous activities if they are relatively symptom-free following manipulation of the cuboid (3)
Cuboid Syndrome: A Typical Plan
Manipulation- Cuboid Whip
Begin with the patient lying face down, knee bent 70° - 90°, and the ankle in a neutral position. Interlock your fingers over the top of the foot, with your thumbs positioned on the underside of the cuboid bone, while applying pressure from above. The patient’s leg must remain fully relaxed during this procedure. While maintaining downward pressure on the cuboid, extend the knee, plantarflex the foot, and rotate the subtalar joint outward. A sudden thrust is delivered to the cuboid bone just before the end range of motion. This manipulation should be executed with speed and firmness, akin to attempting to tear a piece of tissue paper from a roll quickly. An audible sound may sometimes accompany this maneuver.
Therapeutic Modalities
Therapeutic modalities alone are insufficient to facilitate the patient’s return to activity and prevent a reoccurrence of cuboid syndrome. (4) Ultrasound and ice may limit inflammation in the surrounding tissues.
Therapeutic Exercises
The therapeutic exercises should focus on stretching a tight peroneus longus and triceps surae, strengthening the intrinsic and extrinsic muscles of the foot, and proprioception through neuromuscular control exercises. (4) Vele’s exercise is popular for strengthening foot muscles and improving balance. Consider incorporating this exercise, which is already in ChiroUp, into your next treatment plan.
Begin standing near a wall for stability. Stand with your feet shoulder-width apart. Keeping your body straight, bend at the ankles to shift your weight forward onto your toes until your heels are about to lift off the floor. Return to the start position.
Ready to transform your diagnoses into exceptional patient care?
ChiroUp subscribers can dive into an extensive Condition Reference library featuring comprehensive best-practice summaries for over 150 conditions, including Cuboid Syndrome. We’re honored to be your partner in automating clinical excellence! Together, we will become the undeniable best choice for patients and payors alike!
Not yet a ChiroUp subscriber? Click the button below to start accessing up-to-date resources like these at your fingertips!
-
Newell S.G., Woodle A. (1981) Cuboid Syndrome. Physician and Sports Medicine 9, 71-76
Jennings J, Davies GJ. Treatment of cuboid syndrome secondary to lateral ankle sprains: a case series. Journal of orthopaedic & sports physical therapy. 2005 Jul;35(7):409-15. Link
Patterson SM. Cuboid syndrome: a review of the literature. J Sports Sci Med. 2006 Dec 15;5(4):597-606. PMID: 24357955; PMCID: PMC3861761.
Mooney M., Maffey-Ward L. (1994) Cuboid plantar and dorsal subluxations: assessment and treatment. Journal of Orthopedic and Sports Physical Therapy 20(4), 220-226