Chiropractic Care for Children: Safety, Utilization, and Outcomes
It’s a common scenario: a parent walks into your clinic, holding their child’s hand, and asks, “Can chiropractic help kids?” As pediatric musculoskeletal complaints rise, chiropractors are increasingly called upon to provide safe, evidence-informed care for younger patients. This review summarizes the current pediatric chiropractic research, including chiropractic safety in children, utilization, and the most common conditions chiropractors manage.
Chiropractic Safety in Children
Before exploring outcomes, it’s essential to address the question every parent asks first: Is pediatric chiropractic safe for children? The evidence indicates that when delivered by trained clinicians using age-appropriate techniques, pediatric chiropractic care is generally safe. Reported adverse events are uncommon and typically mild, such as brief soreness or temporary irritability, like increased crying.
Moderate or severe reactions appear to be extremely rare, although their exact frequency is uncertain due to the limited availability of high-quality data. Still, multiple reviews and surveys consistently report no pattern of significant harm and an overall very low risk when chiropractors conduct proper screening and use gentle, pediatric-specific methods. (1-4)
Utilization Trends for Chiropractic Care in Children and Adolescents
When considering the question ‘how common is chiropractic care among children?’ current utilization trends indicate that chiropractic care is the leading complementary health service for U.S. children, reflecting its growing role in family healthcare. (5)
National and international surveys indicate that between 3% and 11% of children (ages 4-17) receive pediatric chiropractic care, with adolescents being the most frequent users. Most pediatric chiropractic visits involve musculoskeletal complaints such as back or neck pain, postural problems, or sports injuries. (6-10)
Chiropractic and Pediatrics Research in Action: ChiroUp subscribers can use the childhood pain infographic from the Forms Library to quickly show parents and social media followers the prevalence of childhood pain and the value of chiropractic care.
Musculoskeletal Conditions
For anyone wondering what conditions pediatric chiropractors can treat, musculoskeletal problems remain the most common reason children and adolescents seek care, and the evidence supporting the benefits of pediatric chiropractic continues to expand. These conditions fall squarely within the wheelhouse of most evidence-based chiropractors, who manage them confidently and effectively using established, conservative approaches.
1. Low Back Pain
Musculoskeletal pain is a leading reason for pediatric chiropractic visits. A 2024 RCT of adolescents with low back pain found that adding spinal manipulation (1–2x/week for 12 weeks) to an exercise program significantly improved pain compared to exercise alone. (11)
2. Recurrent Headaches
Chiropractic spinal manipulation may offer relief for children with tension-type or recurrent headaches. A 2021 RCT of 199 children (ages 7–14) showed that spinal manipulation reduced headache days over a 4-month timeframe, with significantly greater global perceived improvement. (12) While headache intensity didn't change between groups, frequency and quality of life were notably better, and side effects were minimal.
Smaller case reports have also noted benefits in pediatric migraines and cervicogenic headaches, though these lack the rigor of RCTs. (13)
3. Adolescent Idiopathic Scoliosis
A 2024 RCT found that adding spinal mobilization to scoliosis treatment sessions reduced curvature and scoliosis-related symptoms in the short term. (14) Similarly, a prospective study by Morningstar et al. (2017) reported stabilization or improvement in 90% of adolescents undergoing chiropractic rehabilitation for scoliosis. (15)
4. Sports Injuries and Overuse Syndromes
The growing popularity of youth athletics has brought a parallel rise in pediatric sports injuries. Injury rates climb proportionally as young athletes spend more time training and competing - often focusing on a single sport at an earlier age. (16-18) The combination of repetitive motion, limited rest, and uneven strength development creates fertile ground for overuse syndromes involving tendons, muscles, and joints.
Chiropractors are well-equipped to manage these issues through manual therapies, targeted rehabilitation, functional screening, and kinetic-chain assessment. By addressing the mechanical and myofascial contributors to overuse, chiropractors deliver meaningful pediatric chiropractic benefits, helping to resolve pain while guiding safe training progression and reducing the risk of recurrence.
💡 Deeper Dive: If you manage active kids and teens, download the Pediatric Sports Injuries Toolkit, an evidence-based resource built to help chiropractors streamline pediatric evaluation, treatment planning, and return-to-play decisions.
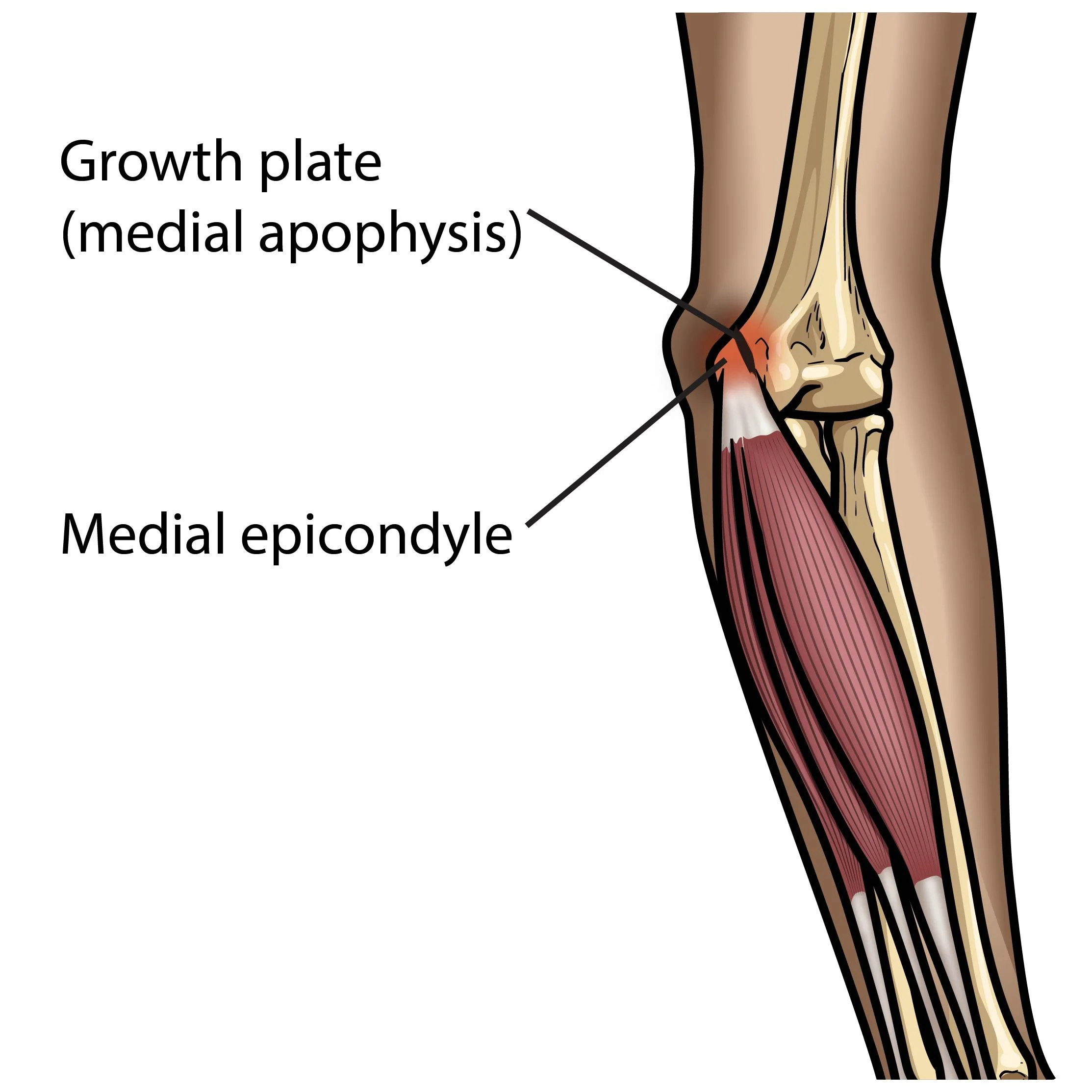
5. Traction Apophysitis (Growth Plate Overuse Injuries)
Traction apophysitis represents a distinct but related category of pediatric overuse injuries, including conditions such as Osgood-Schlatter disease (tibial tuberosity), Sever’s disease (calcaneus), and Little League elbow (medial epicondyle). These disorders are unique to growing athletes because open growth plates are the weakest link in the mechanical chain. Excessive or repetitive load, often associated with increased training volume, irritates these developing attachment sites, resulting in pain and inflammation.
While there is limited high-quality research directly related to the benefits of pediatric chiropractic management for these disorders, the current standard of care emphasizes the same evidence-based strategies chiropractors routinely provide: selective rest and activity modification, structured rehabilitation to restore strength and flexibility, use of orthotics, supports, or braces when indicated, therapeutic modalities to reduce pain and inflammation, and hands-on management of the myofascial and joint restrictions that contribute to abnormal load distribution throughout the kinetic chain. (19-24).
💡 Chiroup subscribers can access their condition reference database to view the associated best practice management protocols for various pediatric traction apophysites:
6. Postural Syndromes
Modern lifestyles have introduced a new epidemic of postural problems among children and teens. Hours spent hunched over devices or seated in class promote the development of upper crossed and lower crossed syndromes, patterns characterized by muscle tightness, inhibition, and joint restriction. These foundational postural imbalances contribute to a range of downstream issues, from spinal pain to decreased physical and mental performance. (25-29)
Contributing factors, such as hyperpronation, weak gluteal activation, and poor core stability, further destabilize the kinetic chain. In essence, many adolescents are building powerful extremities on unstable cores - like firing a cannon from a rowboat instead of a battleship. Chiropractors are skilled at identifying and correcting these dysfunctions through manual therapy, neuromuscular re-education, and corrective exercise, helping young patients build a stronger foundation for lifelong spinal health and performance.
💡 ChiroUp subscribers can download the lower-extremity injury infographic in the Forms Library for a fast clinical reference on common pediatric patterns and risk factors.
And if you want a deeper dive, check out our on-demand webinar on the three-minute functional exam for a quick way to identify the deficits that drive lower-extremity pain.
Functional or Mixed Conditions
Beyond musculoskeletal complaints, many families seek chiropractic input for functional or non-musculoskeletal conditions, where current research on the benefits of pediatric chiropractic remains mixed—often promising, occasionally inconclusive—but clinical experience still guides thoughtful, conservative care.
These presentations are more commonly managed by family-practice or pediatric-focused chiropractors, as not all providers are equally comfortable with conditions that currently have less robust research support.
A Note on “Not Supported by the Literature”
When authors conclude that a particular treatment for a specific condition is not supported by the literature, that typically reflects a lack of data, but not necessarily evidence of ineffectiveness. Many safe, conservative therapies begin as clinical observations that later gain validation through more substantial research. Until more studies are available, chiropractors can best serve young patients by maintaining transparency, documenting outcomes, and integrating evidence-informed decision-making into every case.
7. Infantile Colic
Pediatric chiropractic care for colic has yielded mixed results. A 2023 systematic review of manual therapies reported modest improvements in sleep duration and crying duration (30), while another study showed no difference compared to a placebo. (31)
8. Asthma
Several small studies have investigated the use of chiropractic care for pediatric asthma. Some reported subjective improvements in quality of life. (32,33)
Chiropractors often theorize that by addressing thoracic cage restrictions and improving spinal and rib mobility, spinal manipulative therapy may help patients breathe more freely and perceive less respiratory discomfort. (34)
9. Nocturnal Enuresis
A controlled trial from the 1990s found that chiropractic adjustments led to nighttime dryness in 25% of children compared to just 5% in a sham group. (35) While these early results are promising, they have yet to be replicated in larger contemporary studies.
Beyond spinal and pelvic manipulation, attention to pelvic floor function and abdominal pressure management may also play a meaningful role in addressing enuresis. Recent evidence supports pelvic floor training as an effective, non-pharmacologic intervention for improving bladder control and related dysfunctions. (36,37)
For those interested in a deeper exploration of pelvic floor function, Dr. Lindsay Mumma’s book, Your Pelvic Floor Sucks: But It Doesn’t Have To, offers an outstanding resource for both patients and providers. While primarily focused on adult populations, it provides valuable insight into the conservative management of pelvic floor dysfunction.
10. Otitis Media
The pediatric chiropractic research on treating otitis media remains limited. Case series suggest improvement, and one pilot RCT found SMT was a safe option for resolving middle ear fluid. (38,39,44)
11. Oral Ties and Breastfeeding Difficulties
Ankyloglossia (tongue-tie) and other oral ties (tight or short tissue under the tongue, lip, or cheek that restricts movement) can limit tongue mobility and contribute to breastfeeding difficulties. A recent systematic review reported that combining myofunctional therapy with frenectomy (surgical release of the restrictive tissue) yields the best outcomes, improving maternal comfort, infant weight gain, breastfeeding duration, and tongue mobility. While evidence quality is limited, findings support a multimodal approach to optimize outcomes. (40)
In addition to the conditions listed above, many pediatric chiropractors manage a variety of other issues, including developmental or functional movement concerns, positional head asymmetry, gait abnormalities, balance or coordination delays, feeding difficulties in infants, retained or abnormal primitive reflexes, and residual musculoskeletal tension following birth or injury.
A Note from the Author
Clinicians naturally develop deeper expertise in the areas they focus on, train in, and treat most often. In full disclosure, I do not personally manage non-musculoskeletal pediatric conditions—just as I do not personally provide other validated services like acupuncture or dry needling—because I believe real proficiency requires deeper focus on a manageable number of skills.
That said, our ChiroUp team is genuinely interested in seeing the research in these areas continue to evolve. For readers specializing in this work, we welcome any additional robust pediatric chiropractic research studies that we may have missed. Sharing those findings and continually updating best practices helps ensure our profession advances and that our clinical decisions remain grounded in evidence.
Practice Recommendations for Pediatric Chiropractic Care
Chiropractic pediatric care standards have steadily evolved through a series of landmark consensus projects. Hawk et al. first led two foundational Delphi studies in 2009 and 2016, establishing profession-wide best-practice recommendations for treating infants, children, and adolescents. (41,42)
Building on that groundwork, an international Delphi consensus panel published updated best-practice recommendations for chiropractic management of children in 2024. (43) The participants averaged 22 years in practice, and more than half held postgraduate pediatric chiropractic certifications. Their unified goal was to define safe, appropriate, and evidence-informed approaches to caring for patients under the age of 18. Among the most essential practice expectations identified were:
Weigh risks and benefits of all interventions, considering each child’s anatomy, development, and psychosocial context.
Obtain comprehensive informed consent, including parental and, when appropriate, child assent, and document it clearly.
Perform a thorough case history and age-appropriate physical exam, including developmental milestones and screening for red flags.
Modify manual techniques according to a child’s age, size, developmental stage, and flexibility, using the gentlest yet effective approach. This includes adjusting biomechanical force to match the patient’s smaller frame, accounting for the greater flexibility and lesser muscle mass of growing bodies, and ensuring all procedures protect the integrity of the developing skeleton. Techniques should also be tailored to each child’s comfort and individual needs, with an emphasis on gentle, precise, and developmentally appropriate care.
Refer or co-manage promptly when findings suggest pathology or when progress is limited.
Promote overall wellness through guidance on posture, exercise, injury prevention, nutrition, and healthy habits.
Conclusion: What Should Chiropractors Take Away?
Chiropractic care for children is increasingly recognized as a safe and valuable component of conservative healthcare. The most substantial evidence supports its use for musculoskeletal conditions, while other applications continue to be studied as emerging research broadens our understanding.
By combining clinical expertise, clear communication, and rigorous documentation, chiropractors can ensure that pediatric care remains both safe and evidence-driven, helping the next generation grow strong, active, and resilient.
As you apply these principles in your clinic, imagine having a platform that puts the latest evidence-based protocols, clinical decision support, and patient education tools all at your fingertips. ChiroUp empowers chiropractors to stay sharp, streamline care, and confidently manage a wide range of conditions, from musculoskeletal pain to functional disorders, while saving time and enhancing outcomes.
Get started for FREE today with our 14-day trial, or schedule a walkthrough with our team for a full look at how ChiroUp can elevate your practice and support your clinical excellence.
-
1. Corso M, Cancelliere C, Mior S, Taylor-Vaisey A, Côté P. The safety of spinal manipulative therapy in children under 10 years: a rapid review. Chiropractic & manual therapies. 2020 Feb 25;28(1):12. Link
2. Misra SM, Jaber O, Long C. Chiropractic Care in Children: A Review of Evidence and Safety. Clinical pediatrics. 2025 Jul;64(7):1028-32. Link
3. Alcantara J, Ohm J, Kunz D. The safety and effectiveness of pediatric chiropractic: a survey of chiropractors and parents in a practice-based research network. Explore. 2009 Sep 1;5(5):290-5. Link
4. Hawk C, Khorsan R, Lisi AJ, Ferrance RJ, Evans MW. Chiropractic care for nonmusculoskeletal conditions: a systematic review with implications for whole systems research. The Journal of Alternative and Complementary Medicine. 2007 Jun 1;13(5):491-512. Link
5. Black LI, Clarke TC, Barnes PM, Stussman BJ, Nahin RL. Use of complementary health approaches among children aged 4–17 years in the United States: National Health Interview Survey, 2007–2012. National health statistics reports. 2015 Feb 10(78):1. Link
6. Peng T, Chen B, Brown HS, Douphrate D, Janak J, Gabriel KP. National Trends in the expenditure and utilization of chiropractic Care in US children and adolescents from the 2007-2016 medical expenditure panel survey: a cross sectional study. Journal of Manipulative and Physiological Therapeutics. 2021 Oct 1;44(8):591-600. Link
7. Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Link
8. Peng T, Chen B, Gabriel KP. Utilization of chiropractic care in US children and adolescents: a cross-sectional study of the 2012 national health interview survey. Journal of Manipulative and Physiological Therapeutics. 2018 Nov 1;41(9):725-33. Link
9. Black LI, Barnes PM, Clarke TC, Stussman BJ, Nahin RL. Use of yoga, meditation, and chiropractors among US children aged 4-17 years. Washington, DC: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics; 2018 Nov 1. Link
10. Misra SM, Jaber O, Long C. Chiropractic Care in Children: A Review of Evidence and Safety. Clinical pediatrics. 2025 Jul;64(7):1028-32. Link
11. Yu H, Southerst D, Wong JJ, Verville L, Connell G, Ead L, Mior S, Hestbaek L, Swain M, Brunton G, Shearer HM. Rehabilitation of back pain in the pediatric population: a mixed studies systematic review. Chiropractic & Manual Therapies. 2024 May 8;32(1):14. Link
12. Lynge S, Dissing KB, Vach W, Christensen HW, Hestbaek L. Effectiveness of chiropractic manipulation versus sham manipulation for recurrent headaches in children aged 7–14 years-a randomised clinical trial. Chiropractic & Manual Therapies. 2021 Jan 7;29(1):1. Link
13. Alcantara J, Pankonin KJ. Chiropractic care of a pediatric patient with migraine-type headaches: a case report and selective review of the literature. Explore. 2010 Jan 1;6(1):42-6. Link
14. Küçük E, Öten E, Coşkun G. Effects of spinal mobilisation in adolescent idiopathic scoliosis: A randomised controlled trial. Journal of Paediatrics and Child Health. 2024 Nov;60(11):660-8. Link
15. Morningstar MW, Dovorany B, Stitzel CJ, Siddiqui A. Chiropractic rehabilitation for adolescent idiopathic scoliosis: end-of-growth and skeletal maturity results. Clinics and Practice. 2017 Jan 12;7(1):911. Link
16. Jayanthi N, Pinkham C, Dugas L, Patrick B, LaBella C. Sports specialization in young athletes: evidence-based recommendations. Sports health. 2013 May;5(3):251-7. Link
17. Jayanthi N, Kleithermes S, Dugas L, Pasulka J, Iqbal S, LaBella C. Risk of injuries associated with sport specialization and intense training patterns in young athletes: a longitudinal clinical case-control study. Orthopaedic journal of sports medicine. 2020 Jun 23;8(6):2325967120922764. Link
18. Post EG, Trigsted SM, Riekena JW, Hetzel S, McGuine TA, Brooks MA, Bell DR. The association of sport specialization and training volume with injury history in youth athletes. The American journal of sports medicine. 2017 May;45(6):1405-12. Link
19. Gregory B, Nyland J. Medial elbow injury in young throwing athletes. Muscles, ligaments and tendons journal. 2013 Apr;3(2):91. Link
20. Andelman S, DiPrinzio E, Hausman M. Elbow injuries in the pediatric athlete. Annals of Joint. 2018 Mar 23;3(3). Link
21. Bezuglov EN, Tikhonova АА, Chubarovskiy PV, Repetyuk АD, Khaitin VY, Lazarev AM, Usmanova EM. Conservative treatment of Osgood-Schlatter disease among young professional soccer players. International orthopaedics. 2020 Sep;44(9):1737-43. Link
EM. Conservative treatment of Osgood-Schlatter disease among young professional soccer players. International orthopaedics. 2020 Sep;44(9):1737-43. Link
22. Lyng K, Rathleff MS, Dean BJ, Kluzek S, Holden S. Current Management Strategies in Osgood Schlatter: A cross-sectional mixed method study. Scandinavian Journal of Medicine & Science in Sports. 2020 Jun 19. Link
23. Rathleff MS, Thorborg K, Andreucci A, Riel H. Association of Self-Reported Improvement After 4 Weeks and Outcomes After 52 Weeks Among Adolescents With Patellofemoral Pain and Osgood-Schlatter Disease. Orthopaedic Journal of Sports Medicine. 2024 Oct;12(10):23259671241280581. Link
24. Belikan P, Färber LC, Abel F, Nowak TE, Drees P, Mattyasovszky SG. Incidence of calcaneal apophysitis (Sever’s disease) and return-to-play in adolescent athletes of a German youth soccer academy: a retrospective study of 10 years. Journal of Orthopaedic Surgery and Research. 2022 Dec;17(1):1-6. Link
25. de-la-Iglesia L, Bravo C, Rubí-Carnacea F. Upper crossed syndrome in secondary school students: A mixed-method study. Journal of Taibah University Medical Sciences. 2023 Aug 1;18(4):894-907. Link
26. Zhang C, Zhang J, Yang G. Association between internet addiction and the risk of upper cross syndrome in Chinese college students: A cross sectional study. Medicine. 2023 Jul 28;102(30):e34273. Link27. Warda DG, Nwakibu U, Nourbakhsh A. Neck and upper extremity musculoskeletal symptoms secondary to maladaptive postures caused by cell phones and backpacks in school-aged children and adolescents. InHealthcare 2023 Mar 10 (Vol. 11, No. 6, p. 819). MDPI. Link
28. Dop D, Pădureanu V, Pădureanu R, Niculescu SA, Drăgoescu AN, Moroșanu A, Mateescu D, Niculescu CE, Marcu IR. Risk factors involved in postural disorders in children and adolescents. Life. 2024 Nov 12;14(11):1463. Link
29. Tsang, S.M., Cheing, G.L., Lam, A.K., Siu, A.M., Pang, P.C., Yip, K.C., Chan, J.W. and Jensen, M.P., 2023. Excessive use of electronic devices among children and adolescents is associated with musculoskeletal symptoms, visual symptoms, psychosocial health, and quality of life: a cross-sectional study. Frontiers in public health, 11, p.1178769. Link
30. Tanrıverdi DÇ, Karaahmet AY, Bilgiç FŞ. Colic and sleep outcomes of nonpharmacological intervention in infants with infantile colic: systematic review and metaanalysis. Revista da Associação Médica Brasileira. 2023 May 19;69:e20230071. Link
31. Gotlib A, Rupert R. Chiropractic manipulation in pediatric health conditions–an updated systematic review. Chiropractic & osteopathy. 2008 Sep 12;16(1):11. Link
32. Bronfort G, Evans RL, Kubic P, Filkin P. Chronic pediatric asthma and chiropractic spinal manipulation: a prospective clinical series and randomized clinical pilot study. Journal of manipulative and physiological therapeutics. 2001 Jul 1;24(6):369-77. Link
33. Kaminskyj A, Frazier M, Johnstone K, Gleberzon BJ. Chiropractic care for patients with asthma: a systematic review of the literature. The Journal of the Canadian Chiropractic Association. 2010 Mar;54(1):24. Link
34. Balon J, Aker PD, Crowther ER, Danielson C, Cox PG, O'Shaughnessy D, Walker C, Goldsmith CH, Duku E, Sears MR. A comparison of active and simulated chiropractic manipulation as adjunctive treatment for childhood asthma. New England Journal of Medicine. 1998 Oct 8;339(15):1013-20. Link
35. Reed WR, Beavers S, Reddy SK, Kern G. Chiropractic management of primary nocturnal enuresis. Journal of manipulative and physiological therapeutics. 1994 Nov 1;17(9):596-600. Link
36. Zivkovic V, Lazovic M, Vlajkovic M, Slavkovic A, Dimitrijevic L, Stankovic I, Vacic N. Diaphragmatic breathing exercises and pelvic floor retraining in children with dysfunctional voiding. Eur J Phys Rehabil Med. 2012 Sep 1;48(3):413-21. Link
37. Cammisa I, Zona M, Ferrara P. Management of nocturnal enuresis in children. Minerva pediatrics. 2025. Link
38. Fysh PN. Chronic recurrent otitis media: case series of five patients with recommendations for case management. J Clin Chiropr Pediatr. 1996;1:66-78.
39. Pohlman KA, Holton-Brown MS. Otitis media and spinal manipulative therapy: a literature review. Journal of Chiropractic Medicine. 2012 Sep 1;11(3):160-9. Link
40. Gonzalez Garrido, M.D.P., Garcia-Munoz, C., Rodriguez-Huguet, M., Martin-Vega, F.J., Gonzalez-Medina, G. and Vinolo-Gil, M.J., 2022. Effectiveness of myofunctional therapy in ankyloglossia: a systematic review. International journal of environmental research and public health, 19(19), p.12347. Link
41. Hawk C, Schneider M, Ferrance RJ, Hewitt E, Van Loon M, Tanis L. Best practices recommendations for chiropractic care for infants, children, and adolescents: results of a consensus process. Journal of manipulative and physiological therapeutics. 2009 Oct 1;32(8):639-47. LInk
42. Hawk C, Schneider MJ, Vallone S, Hewitt EG. Best practices for chiropractic care of children: a consensus update. Journal of manipulative and physiological therapeutics. 2016 Mar 1;39(3):158-68. Link
43. Keating, G., Hawk, C., Amorin-Woods, L., Amorin-Woods, D., Vallone, S., Farabaugh, R., Todd, A., Ferrance, R., Young, J., O'Neill Bhogal, S. and Sexton, H., 2024. Clinical practice guideline for best practice management of pediatric patients by chiropractors: results of a delphi consensus process. Journal of Integrative and Complementary Medicine, 30(3), pp.216-232. Link
44. Sawyer CE, Evans RL, Boline PD, Branson R, Spicer A. A feasibility study of chiropractic spinal manipulation versus sham spinal manipulation for chronic otitis media with effusion in children. Journal of manipulative and physiological therapeutics. 1999 Jun 1;22(5):292-8. Link