Cervical Disc Replacement: A Chiropractic Perspective
“The most uneducated person in healthcare—the patient; makes the most important decision—the provider they see first.”
Choosing between disc replacement surgery and fusion surgery can be influenced by six key factors that surgeons consider. It's important to note that surgeons may have a range of surgical options available to them, and their decision often depends on their expertise and the specific procedure they aim to perform. In such cases, choosing the right surgeon becomes as crucial as selecting the most suitable surgical approach.
Don't forget: Your referral and patient education may directly influence the procedure your patient receives.
6 Factors Impacting Your Surgical Referral
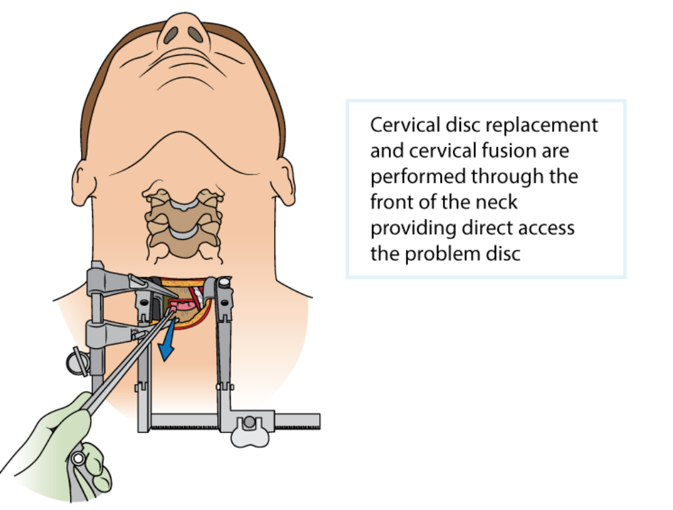
When considering the best surgical approach for your patients with cervical disc issues, chiropractors must weigh the advantages of cervical artificial disc replacement (ADR) against the more traditional anterior cervical discectomy and fusion (ACDF) surgery. Each procedure has unique benefits, but let us use research to make a compelling case for disc replacement surgery.
1. Greater Mobility
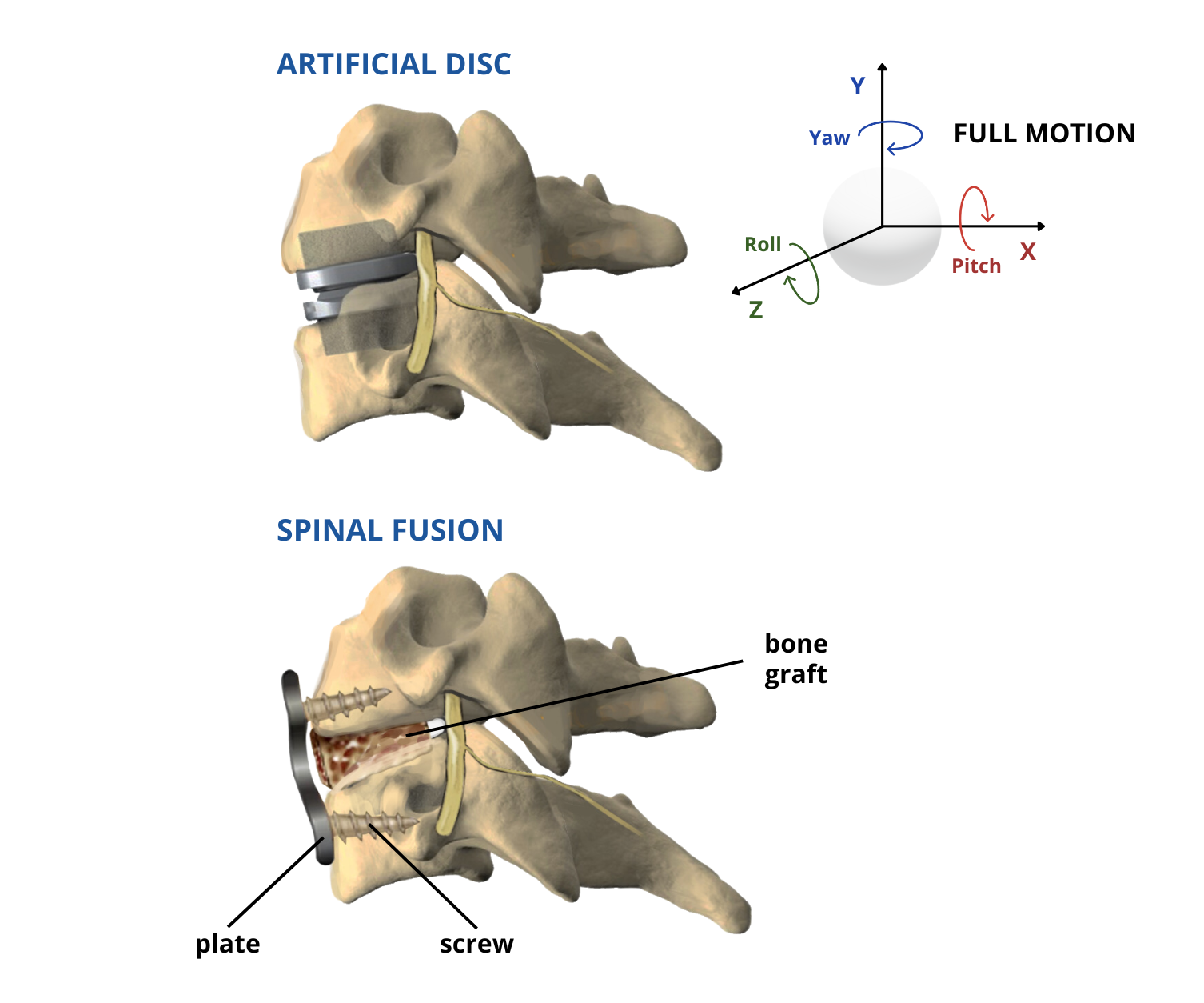
Disc replacements mimic the natural discs in the body. They enable greater spine mobility, allowing patients to move as usual. In contrast, ACDF surgery fuses bones, eliminating movement in the affected spine area.
2. Maintain Natural Biomechanics
Cervical ADR stands apart from ACDF as it maintains motion between the vertebrae rather than fusing them. Some studies suggest that cervical ADR preserves more natural biomechanics in the cervical spine and puts less stress on the discs above and below the surgical site than ACDF. The initial research is promising, but the long-term effects need to be better established.
3. Comparable Clinical Outcomes
ACDF and cervical disc replacement tend to yield favorable clinical outcomes, with success rates exceeding 70% for eligible patients suffering from degenerative disc disease at a single spinal level. Cervical ADR has shown at least equivalent results to ACDF in relieving neck and arm pain and improving patient function and satisfaction, all without increasing surgical complications. (1-3)
4. No Bone Graft-Related Risks
Unlike ACDF, cervical ADR surgery eliminates the need for bone grafts. Bone grafts sometimes fail to heal or fuse properly, resulting in complications. Furthermore, there is no risk of ongoing pain in the patient's pelvis (a common area for harvest).
5. Faster Recovery
Patients undergoing cervical ADR and ACDF can return to light work and most daily activities within about a week post-surgery. However, cervical ADR patients tend to be cleared for more strenuous activities around six weeks after the procedure, whereas ACDF patients may require three months or longer for the fusion to heal. Additionally, while present in both types of surgery, postoperative swallowing difficulties tend to resolve more favorably in cervical disc replacement. (4)
6. Reduced Risk of Adjacent Segment Disease
Artificial discs have demonstrated the ability to maintain and not increase the range of motion postoperatively. Theoretically, this can reduce load transfer and degeneration in the adjacent discs. Some studies suggest that cervical ADR has a lower risk of requiring a repeat or second surgery than ACDF, although more long-term studies are needed to confirm this.
While these benefits may seem relatively minor in some cases, especially when addressing a single level of spinal degeneration, they collectively present a compelling argument in favor of cervical ADR. Importantly, they offer potential advantages for your patients that can lead to improved outcomes and satisfaction.
It's important to acknowledge that, like any surgical procedure, both cervical ADR and ACDF carry some risks and potential complications. However, the advantages of greater mobility, natural biomechanics, and reduced bone graft-related issues make cervical artificial disc replacement a promising choice for your patients.
When should I refer a patient to a surgeon 100% of the time?
Tumor
Fracture
Neurologic Deficit
Cervical Myelopathy
When should I wait to refer?
Axial Back and Neck Pain
Acute Radiculopathy
As you can see, our referral and patient education tools directly influence the procedure your patient receives. It’s our job, as evidence-based chiropractors, to effectively educate our patients about their diagnoses. Unfortunately, patient education can be a tricky.
See how ChiroUp can help you with patient education, communication & compliance HERE.
-
Lavelle WF, Riew KD, Levi A, Florman JE. 10-year Outcomes of Cervical Disc Replacement with the BRYAN® Cervical Disc: Results from a Prospective, Randomized, Controlled Clinical Trial. Spine. 2018.
Burkus JK, Traynelis VC, Haid RW, Mummaneni PV. Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial: Clinical article. J Neurosurg Spine. 2014;21(4):516-28.
Hisey MS, Zigler JE, Jackson R, et al. Prospective, Randomized Comparison of One-level Mobi-C Cervical Total Disc Replacement vs. Anterior Cervical Discectomy and Fusion: Results at 5-year Follow-up. Int J Spine Surg. 2016;10:10.
McAfee PC, Cappuccino A, Cunningham BW, et al. Lower incidence of dysphagia with cervical arthroplasty compared with ACDF in a prospective randomized clinical trial. J Spinal Disord Tech. 2010;23(1):1-8.