7 Essential Neurodynamic Tests For Sciatica And Lumbar Radiculopathies
Nerves are dynamic structures that require the ability to glide and stretch for optimal function. Edema and fibrosis can impair this normal nerve movement, often resulting in neurogenic complaints. Nerve tension tests are crucial for identifying altered neurodynamics and effectively addressing these issues.
Evidence-based chiropractors frequently manage lower extremity radicular pain, with sciatica being the most common culprit. Fortunately, clinicians can accurately identify sciatic nerve involvement through reliable neurodynamic tests, including the Straight Leg Raise (SLR), Braggard, and Slump tests. (1) However, radiculopathies originating above L4 necessitate alternative nerve tension tests.
This blog and video will cover everything you need to master lower extremity neurodynamic testing for all nerves, ensuring your diagnostic accuracy and improving patient outcomes. Don't miss this comprehensive guide to elevating your neurodynamic testing skills!
Neurodynamic testing entails tensioning one or both ends of a selected nerve. The reproduction or increase in neurogenic symptoms indicates a positive test. (2,3) Check out the following synopsis for additional clinical pearls on lower extremity neurodynamic testing.
Sciatica Tests
Straight Leg Raise Test (SLR)
Straight leg raise testing is the most fundamental lower extremity neurodynamic test. The clinician progressively lifts the supine patient's straightened leg until symptoms are reported. Reproducing radicular symptoms in the 30-70 degree range suggests involvement of the L4/5 or L5/S1 nerve roots from radiculopathy or dural irritation. It is also called Lasegue's Test.
Meta-analysis indicates fair reliability (4); a positive straight leg raise test shows 83-89% sensitivity for lumbar radiculopathy. (1,5)
The straight leg raise test shows very low specificity (25%) when performed in isolation. (5)
Increasing patient age is related to a steady decline in the test’s diagnostic accuracy. (6)
Overall test accuracy improves when adding ankle dorsiflexion (aka Braggard test.) (1,4)
Braggard Test
This test is an adjunct after a positive Straight Leg Raise (SLR). Lower the patient's leg 10 degrees below the point of SLR symptom reproduction and dorsiflex the patient's ankle. Reproduction of similar symptoms is a positive test indicating radiculopathy or dural tension.
Combining the Braggard test with the straight leg raise improves sensitivity to 97% for lumbar radiculopathy. (1)
Adding ankle inversion to the Braggard test can help differentiate peroneal (fibular) nerve involvement.
Adding ankle eversion to the Braggard test can help differentiate tibial nerve involvement.
Differentiating lumbar radiculopathies from hamstring strains can be challenging; however, Braggard test can help, as hamstring symptoms typically remain unaffected by this maneuver, while lumbar spine issues may be exacerbated. (7)
Extended Straight Leg Raise Test (ESLR)
The clinician progressively lifts the supine patient’s straightened leg until radicular symptoms are reported (SLR). The clinician then performs ankle dorsiflexion to increase neural tension for thigh symptoms or hip internal rotation to increase neural tension for lower leg symptoms. Exacerbation of radicular complaints upon dorsiflexion or hip rotation suggests a neurologic origin vs. a musculoskeletal origin. (8)
The Extended Straight Leg Raise increases tension on remote neural structures without affecting local musculoskeletal tissues.
For proximal symptoms (above the knee), ankle dorsiflexion (Braggard test) is applied to enhance neural tension below the knee without affecting the MSK tissues below the knee.
For patients with distal symptoms (below the knee), hip internal rotation is applied to increase neural tension above the knee without affecting the MSK tissues below the knee.
The Extended Straight Leg Raise is a reliable and reproducible test. (8)
Crossed Straight Leg Raise Test (XSLR)
The crossed straight leg raise test is simply a standard straight leg raise that reproduces symptoms in the opposite lower extremity—it is also called the Well Leg Raise or Fajersztajn sign.
Reported to be associated with a herniated lumbar disc in 97% of patients. (9)
It may predict a poor response to conservative management. (9)
Reliability estimates are wide-ranging. (4)
Modified Slump Test
The modified slump test combines several provocative neural tension maneuvers into a single test by concurrently performing a seated bilateral SLR with ankle dorsiflexion, trunk & neck flexion with practitioner overpressure, and a Valsalva maneuver. Reproduction of lower extremity complaints suggests radiculopathy or dural tension.
The ultimate lower extremity neurodynamic tension test.
A negative modified slump test means the following tests are also likely negative: straight leg raise, crossed straight leg raise, Bechterews test, Braggard test, Valsalva, and Soto-hall.
A negative modified slump test “is effective in dismissing lumbar or lumbosacral radiculopathy.” (1)
Femoral Nerve Radiculopathy Tests
While initial studies estimated the prevalence of mid and upper-lumbar nerve root impingement to be between 5% and 11%, more recent research on lumbar disc herniation indicates that this condition may be significantly more common. (10)
While the above-mentioned tests effectively identify lower lumbar radiculopathies, diagnosing mid and upper-lumbar radiculopathies requires alternative assessments, including the following tests.
Femoral Nerve Stretch Test (FNST)
The clinician grasps the prone patient's ankle on the symptomatic side and facilitates gentle passive knee flexion; reproduction of typical lower extremity pain suggests femoral radiculopathy. (10,11)
Used to assess mid or high-lumbar radiculopathy (i.e., L2-4)
Reported to be positive in 84% to 95% of patients with mid or upper-lumbar discs. (12-15)
It is also strongly associated with a lateral disc protrusion at the L4/5 level. (14)
The test was initially described principally as prone knee flexion; however, adding hip extension improves sensitivity and reliability (16,17)
It may yield false positives due to tight or injured anterior thigh muscles, as well as hip bone or joint issues. (12)
Crossed Femoral Nerve Stretch Test (XFNST)
The clinician grasps the prone patient's ankle on the asymptomatic side and facilitates gentle passive knee flexion. Reproduction of contralateral (symptomatic) lower extremity pain leg suggests femoral radiculopathy. (10)
The crossed femoral nerve stretch test may be a valuable screening test supporting a diagnosis of upper lumbar radiculopathy. (12)
Advanced Approaches: Mastering the Treatment of Sciatic and Femoral Nerve Radiculopathies
Nerve tension testing involves stretching both ends of a nerve to its maximum capacity. It is primarily used for diagnostic purposes and occasionally in the later stages of rehabilitation.
In contrast, nerve flossing alternates between tensioning one end of the nerve and releasing tension on the other end. This back-and-forth motion helps the nerve glide smoothly through its path, aiming to break down adhesions that may have formed. Therapeutic nerve flossing can be conducted by a clinician in-office or incorporated into a home-based exercise program.
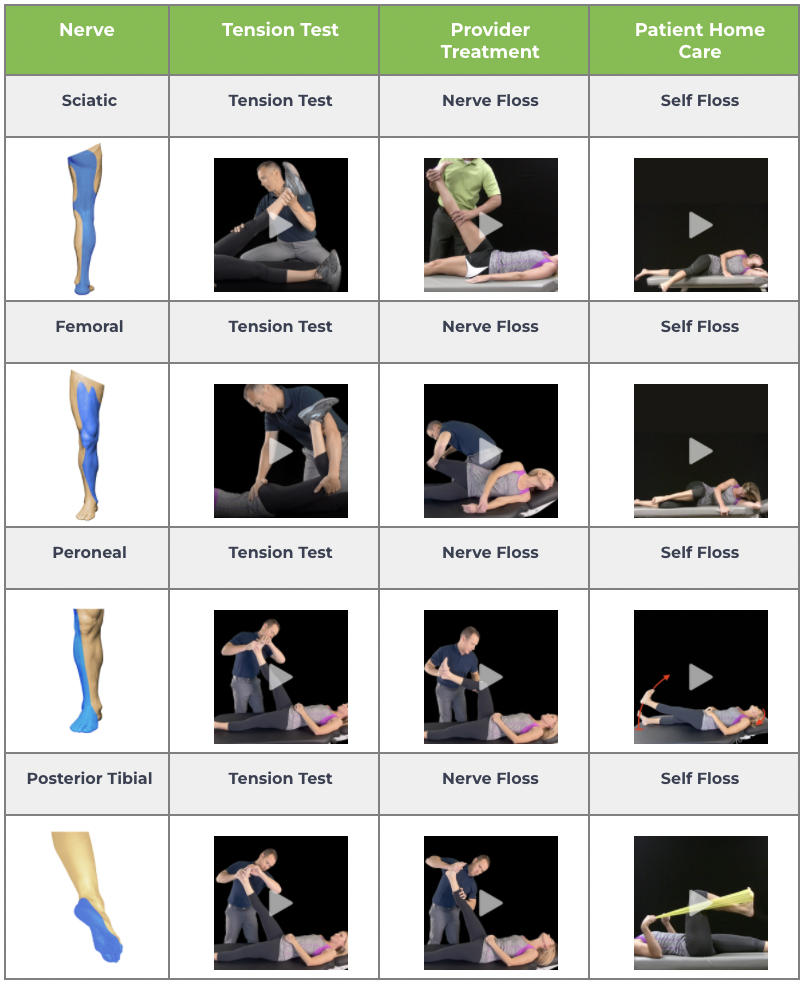
Check out the following chart of practical in-office and home nerve flossing exercises designed to enhance your clinical outcomes for lower extremity issues. ChiroUp subscribers can review any of the associated clinical videos in their clinical skills library.
Experience the difference with ChiroUp. Our platform is tailor-made to enhance your clinical skills, ensuring you deliver the pinnacle of care to every patient, every time.
Join the ranks of thousands of chiropractors who are transforming the landscape of chiropractic care. Take the next step toward excellence.
-
1. González Espinosa de los Monteros FJ, Gonzalez-Medina G, Ardila EM, Mansilla JR, Expósito JP, Ruiz PO. Use of neurodynamic or orthopedic tension tests for the diagnosis of lumbar and lumbosacral radiculopathies: study of the diagnostic validity. International Journal of Environmental Research and Public Health. 2020 Oct;17(19):7046. Link
2. Butler D. The sensitive nervous system. Adelaide: Noigroup Publications; 2000.
3. Shacklock M. Clinical neurodynamics: a new system of neuromusculoskeletal treatment. Elsevier Health Sciences; 2005 May 6.
4. Nee RJ, Coppieters MW, Boyd BS. Reliability of the straight leg raise test for suspected lumbar radicular pain: A systematic review with meta-analysis. Musculoskeletal Science and Practice. 2022 Jun 1;59:102529. Link
5. Montaner-Cuello A, Bueno-Gracia E, Rodríguez-Mena D, Estébanez-de-Miguel E, Malo-Urriés M, Ciuffreda G, Caudevilla-Polo S. Is the Straight Leg Raise Suitable for the Diagnosis of Radiculopathy? Analysis of Diagnostic Accuracy in a Phase III Study. InHealthcare 2023 Dec 11 (Vol. 11, No. 24, p. 3138). MDPI. Link
6. Qazi SA, Qazi RA, Ahmed T, Rehman L, Javeed F, Aziz HF. The diagnostic accuracy of straight leg raise test in patients more than 60 years of age suffering lumbar disk herniation with low back pain and sciatica. Journal of Neurosciences in Rural Practice. 2023 Oct;14(4):610. Link
7. Bueno-Gracia E, Pérez-Bellmunt A, Estébanez-de-Miguel E, López-de-Celis C, Shacklock M, Caudevilla-Polo S, González-Rueda V. Differential movement of the sciatic nerve and hamstrings during the straight leg raise with ankle dorsiflexion: Implications for diagnosis of neural aspect to hamstring disorders. Musculoskeletal Science and Practice. 2019 Oct 1;43:91-5. Link
8. Pesonen, J., Shacklock, M., Rantanen, P. et al. Extending the straight leg raise test for improved clinical evaluation of sciatica: reliability of hip internal rotation or ankle dorsiflexion. BMC Musculoskelet Disord 22, 303 (2021) Link
9. Hudgins RW. The crossed straight leg raising test: a diagnostic sign of herniated disc. Journal of Occupational and Environmental Medicine. 1979 Jun 1;21(6):407-8. Link
10. Suri P, Rainville J, Katz JN, Jouve C, Hartigan C, Limke J, Pena E, Li L, Swaim B, Hunter DJ. The accuracy of the physical examination for the diagnosis of midlumbar and low lumbar nerve root impingement. Spine. 2011 Jan 1;36(1):63-73. Link
11. Randelli F, Pace F, Maglione D, Capitani P, Sampietro M, Favilla S. Differential Diagnosis of Hip Pain. Diagnosis and Management of Femoroacetabular Impingement: An Evidence-Based Approach. 2017:5-26. Link
12. Nadler SF, Malanga GA, Stitik TP, Keswani R, Foye PM. The crossed femoral nerve stretch test to improve diagnostic sensitivity for the high lumbar radiculopathy: 2 case reports. Archives of physical medicine and rehabilitation. 2001 Apr 1;82(4):522-3. Link
13. Porchet F, Fankhauser H, De Tribolet N. Extreme lateral lumbar disc herniation: clinical presentation in 178 patients. Acta neurochirurgica. 1994 Sep;127:203-9. Link
14. Christodoulides AN. Ipsilateral sciatica on femoral nerve stretch test is pathognomonic of an L4/5 disc protrusion. The Journal of Bone & Joint Surgery British Volume. 1989 Jan 1;71(1):88-9. Link
15. Abdullah AF, Wolber PG, Warfield JR, Gunadi KI. Surgical management of extreme lateral lumbar disc herniations: review of 138 cases. Neurosurgery. 1988 Apr 1;22(4):648-53. Link
16. Geraci MC, Alleva JT, McAdam FB. Physical examination of the spine and its functional kinetic chain. The low back pain handbook. Philadelphia: Hanley and Belfus. 1997:49-70. Link
17. Penning L, Wilmink JT. Biomechanics of lumbosacral dural sac: a study of flexion-extension myelography. Spine. 1981 Jul 1;6(4):398-408. Link