Chiropractors: 10 Things to Know About Pelvic Floor Dysfunction
Reading time: 3 minutes
Pelvic floor dysfunction significantly impacts the quality of life in up to 1 in 4 women. Problems range from stress incontinence to inadequate core stability and chronic back pain. Unfortunately, many chiropractors have a limited skillset for this ubiquitous problem.
ChiroUp’s newest protocol summarizes the current best-practice management for this condition, including expert advice from more than a dozen providers who treat and teach pelvic floor dysfunction.
Want the down and dirty?
Check out this one-minute video synopsis of the docs sharing what they know about pelvic floor problems.
Want more?
Check out our top ten clinical pearls from our newest protocol:
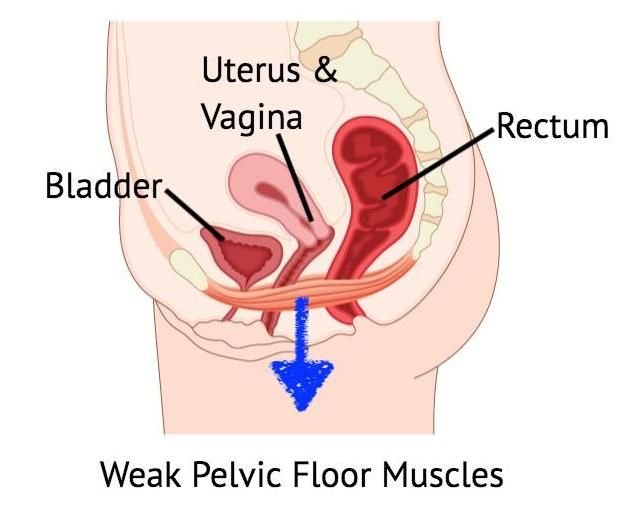
1. The Problem
Dysfunction can arise when the pelvic floor’s muscular hammock is excessively stretched, damaged, or otherwise weakened- leading to stiff and distensile fibers that cannot generate power and sustained contraction. (15) Conversely, pelvic floor muscles can become hypertonic and overactive, causing rapid fatigue. (15)
2. Risks
Vaginal childbirth is the primary risk factor for pelvic floor dysfunction. More than 90% of women demonstrate some form of pelvic floor injury following vaginal childbirth. (24)
3. Symptoms
Pelvic floor dysfunction presents as a complex clinical picture with a spectrum of potential symptoms, including pain, urinary urgency or incontinence, fecal urgency or incontinence, sexual dysfunction, and pelvic organ prolapse. (2,14,34)While females account for 95% of pelvic floor presentations, males are not immune and can experience symptoms including chronic pain, prostatitis, and sexual dysfunction. (16,19,20)
4. Assessment
Like any other muscle dysfunction syndrome, management hinges on identifying hypotonicity vs. hypertonicity as the primary culprit.
Manual therapists should carefully consider whether they are the best-suited clinician for the hands-on assessment. Before embarking on any palpatory evaluation of the pelvic floor, examiners must weigh many factors, including your scope of practice, training, informed consent, patient expectations, gender preferences, and liability issues. (A specialty-trained pelvic floor physical therapist is the most common type of practitioner to perform an internal pelvic floor evaluation.) (82)
5. Management
Patients with weak or hypotonic vaginal and anal muscles may benefit from Kegel-type exercises. In contrast, those with hypertonicity might be better served by techniques like manual therapy, scar tissue manipulation, modalities (ultrasound, e-stim, ESWT), massage, dilators, breathing re-training, cognitive behavioral therapy, and meditation. (42,44)
6. Kegels
In cases of pelvic muscle weakness, Kegel exercises may be appropriate. Proper instruction and exercise monitoring are essential, as most women with pelvic floor dysfunction have an inaccurate self-perception of pelvic floor muscle contraction. (61) Many patients will often incorrectly bear down, performing a Valsalva maneuver instead of a Kegel. Monitoring devices or internal self-assessment by the patient can confirm a proper lift and squeeze technique.
7. Alternatives
One of the quandaries for prescribing Kegel exercises is that a hands-on pelvic exam is a prerequisite; however, very few practitioners are qualified and willing to provide that service. Fortunately, core and eccentric pelvic floor training exercises are alternatives to Kegel exercises that may benefit patients with either hypertonicity or hypotonicity.
8. Rehab Benefits
Pelvic floor muscle training performed for three months can lead to significant quality of life improvements. (62) Women who perform pelvic floor muscle training are five times more likely to report resolution of urinary incontinence. (58)
9. Aerobic Exercise
Concurrent general aerobic training may enhance outcomes for pelvic floor rehab. (55,64) Regular aerobic exercise may also help maintain improvements achieved through pelvic muscle training. (42) Incorporating Pilates and yoga may be useful adjuncts. (65)
10. Patient Education
Patient education is a crucial component of recovery. (26) Considerations include:
Providing a potent rationale and motivation for home exercise.
Teaching controlled fluid intake and timed urination skills, although some patients may not respond to bladder training. (36) The natural tendency to avoid fluids can lead to dehydration and subsequent muscle dysfunction.
Patients must understand the importance of diet, including limiting caffeine, alcohol, artificial sweeteners, and inflammatory or gas-producing foods. (66)
Most importantly, providers must provide an environment of support, empathy, and compassion so that patients are comfortable discussing their concerns.
Want to put this information into action?
Subscribers can visit the condition reference library to review the entire new protocol, including all assessments, treatments, and exercises. Plus, subscribers can relay the essential exercises and ADLs to their patients with a couple of clicks. Get started now!
-
Shannon MB, Mueller ER. Pelvic Pain Associated with a Gynecologic Etiology. InPelvic Floor Disorders 2021 (pp. 879-889). Springer, Cham.
Reiner CS, Schawkat K. Dynamic Magnetic Resonance Imaging of Pelvic Floor Pathologies. InPelvic Floor Disorders 2021 (pp. 653-660). Springer, Cham. Link
Bedretdinova D, Fritel X, Zins M, Ringa V. The effect of urinary incontinence on health-related quality of life: is it similar in men and women?. Urology. 2016 May 1;91:83-9. Link
Jantos M. A Myofascial Perspective on Chronic Urogenital Pain in Women. InPelvic Floor Disorders 2021 (pp. 923-943). Springer, Cham. Link
Dieter AA, Wilkins MF, Wu JM. Epidemiological trends and future care needs for pelvic floor disorders. Current opinion in obstetrics & gynecology. 2015 Oct;27(5):380. Link
Messelink B, Benson T, Berghmans B, Bo K, Corcos J, Fowler C, Laycock J, Lim PH, van Lunsen R, Nijeholt GA. Standardization of terminology of pelvic floor muscle function and dysfunction: report from the pelvic floor clinical assessment group of the International Continence Society. Neurourology and urodynamics. 2005 Jan 1;24(4):374. Link
Theodorsen NM, Strand LI, Bø K. Effect of pelvic floor and transversus abdominis muscle contraction on inter-rectus distance in postpartum women: a cross-sectional experimental study. Physiotherapy. 2019 Sep 1;105(3):315-20. Link
Continence Foundation of Australia. 2018. Pelvic Floor Muscles in Men. Accessed 3/12/2021 from: Link
10 . Foundation Physiotherapy. 2018. 5 Basic Functions of your Pelvic Floor. Accessed 03/12/2021 from: Link
Theodorsen NM, Strand LI, Bø K. Effect of pelvic floor and transversus abdominis muscle contraction on inter-rectus distance in postpartum women: a cross-sectional experimental study. Physiotherapy. 2019 Sep 1;105(3):315-20. Link
The Male Pelvic Floor. Physiopedia. Accessed 03/1/2021 from: Link
Lowenstein L, Gruenwald I, Gartman I, Vardi Y. Can stronger pelvic muscle floor improve sexual function? International Urogynecology Journal. 2010 May;21(5):553-6. Link
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008 Sep 17;300(11):1311-6. Link
Marques A, Stothers L, Macnab A. The status of pelvic floor muscle training for women. Canadian Urological Association Journal. 2010 Dec;4(6):419. Link
Cohen D, Gonzalez J, Goldstein I. The role of pelvic floor muscles in male sexual dysfunction and pelvic pain. Sexual medicine reviews. 2016 Jan 1;4(1):53-62. Link
Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, Spino C, Whitehead WE, Wu J, Brody DJ, Pelvic Floor Disorders Network. Prevalence of symptomatic pelvic floor disorders in US women. Jama. 2008 Sep 17;300(11):1311–6. Link
Harvey MA. Pelvic floor exercises during and after pregnancy: a systematic review of their role in preventing pelvic floor dysfunction. Journal of Obstetrics and Gynaecology Canada. 2003 Jun 1;25(6):487-98. Link
Theodorsen NM, Strand LI, Bø K. Effect of pelvic floor and transversus abdominis muscle contraction on inter-rectus distance in postpartum women: a cross-sectional experimental study. Physiotherapy. 2019 Sep 1;105(3):315-20. Link
Kavvadias T, Baessler K, Schuessler B. Pelvic pain in urogynaecology. Part I: evaluation, definitions and diagnoses. International urogynecology journal. 2011 Apr;22(4):385-93. Link
Shannon MB, Mueller ER. Pelvic Pain Associated with a Gynecologic Etiology. InPelvic Floor Disorders 2021 (pp. 879-889). Springer, Cham.
Berghmans B, Nieman F, Leue C, Weemhoff M, Breukink S, Van Koeveringe G. Prevalence and triage of first contact pelvic floor dysfunction complaints in male patients referred to a Pelvic Care Centre. Neurourology and urodynamics. 2016 Apr;35(4):487-91. Link
Kirby AC, Luber KM, Menefee SA. An update on the current and future demand for care of pelvic floor disorders in the United States. American journal of obstetrics and gynecology. 2013 Dec 1;209(6):584-e1. Link
Nygaard I. New directions in understanding how the pelvic floor prepares for and recovers from vaginal delivery. American Journal of Obstetrics & Gynecology. 2015 Aug 1;213(2):121-2. Link
Quiroz LH, Muñoz A, Shippey SH, Gutman RE, Handa VL. Vaginal parity and pelvic organ prolapse. The Journal of reproductive medicine. 2010 Mar;55(3-4):93. Link
Memon H, Handa VL. Pelvic floor disorders following vaginal or cesarean delivery. Current opinion in obstetrics & gynecology. 2012 Oct;24(5):349. Link
de Almeida BS, Sabatino JH, Giraldo PC. Effects of high-velocity, low-amplitude spinal manipulation on strength and the basal tonus of female pelvic floor muscles. Journal of manipulative and physiological therapeutics. 2010 Feb 1;33(2):109-16. Link
Marques A, Stothers L, Macnab A. The status of pelvic floor muscle training for women. Canadian Urological Association Journal. 2010 Dec;4(6):419. Link
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstetrics & Gynecology. 1997 Apr 1;89(4):501-6. Link
Smith FJ, Holman CA, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstetrics & Gynecology. 2010 Nov 1;116(5):1096-100. Link
Denman MA, Gregory WT, Boyles SH, Smith V, Edwards SR, Clark AL. Reoperation 10 years after surgically managed pelvic organ prolapse and urinary incontinence. American journal of obstetrics and gynecology. 2008 May 1;198(5):555-e1. Link
Fialkow MF, Newton KM, Weiss NS. Incidence of recurrent pelvic organ prolapse 10 years following primary surgical management: a retrospective cohort study. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(11):1483–7.Link
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ open. 2011 Jan 1;1(2).Link
Pedraza R, Nieto J, Ibarra S, Haas EM. Pelvic muscle rehabilitation: a standardized protocol for pelvic floor dysfunction. Advances in urology. 2014 Oct;2014. Link
Cerruto MA. Chronic Pelvic Pain and Chronic Pelvic Pain Syndrome: Classification and Epidemiology. InChronic Pelvic Pain and Pelvic Dysfunctions 2021 (pp. 49-60). Springer, Cham. Link
Mumma, L. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/09/2021.
Pedraza R, Nieto J, Ibarra S, Haas EM. Pelvic muscle rehabilitation: a standardized protocol for pelvic floor dysfunction. Advances in urology. 2014 Oct;2014. Link
Pastore EA, Katzman WB. Recognizing myofascial pelvic pain in the female patient with chronic pelvic pain. Journal of Obstetric, Gynecologic & Neonatal Nursing. 2012 Sep 1;41(5):680-91. Link
Dommerholt J, Bron C, Franssen J. Myofascial trigger points: an evidence-informed review. Journal of Manual & Manipulative Therapy. 2006 Oct 1;14(4):203-21. Link
Simons DG, Travell JG, Simons LS. Travell and Simon’ myofascial pain and dysfunction: The trigger point manual. 2nd ed. Vol. 2. Williams and Wilkins; London: 1999b.
Trigger Point Therapy for Pelvic Pain. Medical College of Wisconsin- Obstetrics & Gynecology Department. Accessed 02/27/2021 from: Link
Howard C. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/04/2021.
Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstetrics and gynecology clinics of North America. 2009 Sep 1;36(3):707-22. Link
Vandyken, C. Pelvic Physiotherapy- to Kegel of Not? Pelvic Health Solutions. Accessed 02/27/21 from: Link
Mennerick E. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/02/2021.
Apte G, Nelson P, Brismée JM, Dedrick G, Justiz III R, Sizer Jr PS. Chronic female pelvic pain—part 1: clinical pathoanatomy and examination of the pelvic region. Pain Practice. 2012 Feb;12(2):88-110. Link
Neville C, Mallinson T, Badillo SA, Fitzgerald CM, Hynes C, Tu F. Comparison of PT and MD Findings of Physical Examination of Patients With and With-out Chronic Pelvic Pain. Journal of Women’s Health Physical Therapy. 2009 Apr 1;33(1):16. Link
Tu FF, Holt J, Gonzales J, Fitzgerald CM. Physical therapy evaluation of patients with chronic pelvic pain: a controlled study. American journal of obstetrics and gynecology. 2008 Mar 1;198(3):272-e1. Link
Navarro Brazález B, Torres Lacomba M, de la Villa P, Sanchez Sanchez B, Prieto Gómez V, Asúnsolo del Barco Á, McLean L. The evaluation of pelvic floor muscle strength in women with pelvic floor dysfunction: a reliability and correlation study. Neurourology and urodynamics. 2018 Jan;37(1):269-77. Link
Ribeiro AM, Nammur LG, Mateus-Vasconcelos EC, Ferreira CH, Muglia VF, Oliveira HF. Pelvic floor muscles after prostate radiation therapy: morpho-functional assessment by magnetic resonance imaging, surface electromyography and digital anal palpation. International braz j urol. 2021 Feb;47(1):120-30. Link
Thompson JA, O’Sullivan PB, Briffa K, Neumann P. Assessment of pelvic floor movement using transabdominal and transperineal ultrasound. International Urogynecology Journal. 2005 Aug;16(4):285-92. Link
Bazzocchi G, Balloni M, Turroni S. Microbiome and Chronic Pelvic Pain. InChronic Pelvic Pain and Pelvic Dysfunctions 2021 (pp. 145-159). Springer, Cham. Link
Apte G, Nelson P, Brismée JM, Dedrick G, Justiz III R, Sizer Jr PS. Chronic female pelvic pain—part 1: clinical pathoanatomy and examination of the pelvic region. Pain Practice. 2012 Feb;12(2):88-110. Link
Butrick CW. Pelvic floor hypertonic disorders: identification and management. Obstetrics and gynecology clinics of North America. 2009 Sep 1;36(3):707-22. Link
Marques A, Stothers L, Macnab A. The status of pelvic floor muscle training for women. Canadian Urological Association Journal. 2010 Dec;4(6):419. Link
Laycock J. Concepts of neuromuscular rehabilitation and pelvic floor muscle training. InPelvic floor re-education 2008 (pp. 177-183). Springer, London. Link
Huang YC, Chang KV. Kegel Exercises. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. 2020 Jan.
Uechi N, Fernandes AC, Bø K, de Freitas LM, de la Ossa AM, Bueno SM, Ferreira CH. Do women have an accurate perception of their pelvic floor muscle contraction? A cross‐sectional study. Neurourology and urodynamics. 2020 Jan;39(1):361-6. Link
Mohktar MS, Ibrahim F, Rozi NF, Yusof JM, Ahmad SA, Yen KS, Omar SZ. A quantitative approach to measure women’s sexual function using electromyography: A preliminary study of the Kegel exercise. Medical science monitor: international medical journal of experimental and clinical research. 2013;19:1159. Link
Marques A, Stothers L, Macnab A. The status of pelvic floor muscle training for women. Canadian Urological Association Journal. 2010 Dec;4(6):419. Link
Uechi N, Fernandes AC, Bø K, de Freitas LM, de la Ossa AM, Bueno SM, Ferreira CH. Do women have an accurate perception of their pelvic floor muscle contraction? A cross‐sectional study. Neurourology and urodynamics. 2020 Jan;39(1):361-6. Link
Fitz FF, Costa TF, Yamamoto DM, Resende AP, Stüpp L, Sartori MG, Girão MJ, Castro RA. Impact of pelvic floor muscle training on the quality of life in women with urinary incontinence. Revista da Associação Médica Brasileira (English Edition). 2012 Mar 1;58(2):155-9. Link
FitzGerald MP, Anderson RU, Potts J, Payne CK, Peters KM, Clemens J, …Nyberg L. Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. The Journal of Urology. 2009;182(2):570–580.
Sapsford RR, Hodges PW. Contraction of the pelvic floor muscles during abdominal maneuvers. Archives of physical medicine and rehabilitation. 2001 Aug 1;82(8):1081-8. Link
Baessler K, Schüssler B, Burgio KL, Moore KH, Norton PA, Stanton SL. Pelvic floor re-education. London: Springer. 2008. Link
Bharucha AE, Chakraborty S, Sletten CD. Common functional gastroenterological disorders associated with abdominal pain. InMayo Clinic proceedings 2016 Aug 1 (Vol. 91, No. 8, pp. 1118-1132). Elsevier. Link
Ayeleke RO, Hay‐Smith EJ, Omar MI. Pelvic floor muscle training added to another active treatment versus the same active treatment alone for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2013(11). Link
NHS., 2021. Urinary Incontinence. [online]. Accessed 3/12/2021 from: Link
Maxwell M, Semple K, Wane S, Elders A, Duncan E, Abhyankar P, Wilkinson J, Tincello D, Calveley E, MacFarlane M, McClurg D. PROPEL: implementation of an evidence based pelvic floor muscle training intervention for women with pelvic organ prolapse: a realist evaluation and outcomes study protocol. BMC health services research. 2017 Dec;17(1):1-0. Link
NHS, 2021. Urinary Incontinence – Accessed 03/04/2021 from: Link
Sapsford R. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Manual therapy. 2004 Feb 1;9(1):3-12. Link
Bø K, Talseth T, Holme I. Single blind, randomised controlled trial of pelvic floor exercises, electrical stimulation, vaginal cones, and no treatment in management of genuine stress incontinence in women. Bmj. 1999 Feb 20;318(7182):487-93. Link
FitzGerald MP, Payne CK, Lukacz ES, Yang CC, Peters KM, Chai TC, Nickel JC, Hanno PM, Kreder KJ, Burks DA, Mayer R. Randomized multicenter clinical trial of myofascial physical therapy in women with interstitial cystitis/painful bladder syndrome and pelvic floor tenderness. The Journal of urology. 2012 Jun;187(6):2113-8. Link
Whooley J, Cunnane EM, Do Amaral R, Joyce M, MacCraith E, Flood HD, O'Brien FJ, Davis NF. Stress urinary incontinence and pelvic organ prolapse: Biologic graft materials revisited. Tissue Engineering Part B: Reviews. 2020 Oct 1;26(5):475-83. Link
Lim R, Liong ML, Leong WS, Khan NA, Yuen KH. Pulsed magnetic stimulation for stress urinary incontinence: 1-year followup results. The Journal of urology. 2017 May 1;197(5):1302-8. Link
But I. Conservative treatment of female urinary incontinence with functional magnetic stimulation. Urology. 2003 Mar 1;61(3):558-61. Link
Yamanishi T, Homma Y, Nishizawa O, Yasuda K, Yokoyama O, SMN‐X study group. Multicenter, randomized, sham‐controlled study on the efficacy of magnetic stimulation for women with urgency urinary incontinence. International Journal of Urology. 2014 Apr;21(4):395-400. Link
Long CY, Lin KL, Lee YC, Chuang SM, Lu JH, Wu BN, Chueh KS, Ker CR, Shen MC, Juan YS. Therapeutic effects of low intensity extracorporeal low energy shock wave therapy (LiESWT) on stress urinary incontinence. Scientific reports. 2020 Apr 2;10(1):1-0. Link
Burgio KL, Robinson JC, Engel BT. The role of biofeedback in Kegel exercise training for stress urinary incontinence. American journal of obstetrics and gynecology. 1986 Jan 1;154(1):58-64. Link
Tries J. Kegel exercises enhanced by biofeedback. Journal of enterostomal therapy. 1990 Mar 1;17(2):67-76. Link
Vickers D, Davila GW. Kegel exercises and biofeedback. InPelvic Floor Dysfunction 2008 (pp. 303-310). Springer, London. Link
Wallace SL, Miller LD, Mishra K. Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Current Opinion in Obstetrics and Gynecology. 2019 Dec 1;31(6):485-93. Link
Connor K.Geletka B. Dry Needling for Pelvic Dysfunction? University Hospitals. February 25, 2020 Accessed 03/16/21 from: https://www.uhhospitals.org/for-clinicians/articles-and-news/articles/2020/02/dry-needling-for-pelvic-dysfunction
Hyde T. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/14/2021.
Tucker J. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/15/2021.
Barry M. RE: “Pelvic Floor Dysfunction Protocol.” Message to Tim Bertelsman regarding advice on chiropractic management of pelvic floor dysfunction patients via direct email on 03/17/2021.
Molander U, Milsom I, Ekelund P, Mellström D. An epidemiological study of urinary incontinence and related urogenital symptoms in elderly women. Maturitas 1990;12(1):51–60. Link
Thom D. Variation in estimates of urinary incontinence prevalence in the community: effects of differences in definition, population characteristics, and study type. J Am Geriatr Soc 1998;46(4):473–480. Link
Wilson L, Brown JS, Shin GP, Luc KO, Subak LL. Annual direct cost of urinary incontinence. Obstet Gynecol 2001;98(3):398–406. Link