10 Facts Every DC Should Know About Leg Length Discrepancy
Reading time: 5 minutes
Most chiropractors routinely identify Leg Length Discrepancy (LLD). But does it matter, and if so, how should we treat it? This blog aims to answer your most important questions regarding the evidence-based management of leg length discrepancy, including:
Can LLD’s cause symptoms?
What is the most straightforward and most accurate test for identifying LLD?
When does an LLD require treatment?
Do I implement a lift all at once or gradually?
At what point is an external heel build-up needed?
Watch the docs evaluate LLD 👇
1. Prevalence of LLD
Up to 90 % of individuals exhibit at least some degree of LLD with a mean inequality of 5.2 mm. (1)
2. Causes of LLD
LLD is categorized into two primary etiologies, with some patients demonstrating a combination of both: (2,3)
Anatomic causes may be congenital (i.e., hip dislocation, etc.) or acquired (i.e., fracture, SCFE, degeneration, surgery, etc.)
Functional origins include muscle imbalances, lower crossed syndrome, hip abductor weakness, foot hyperpronation, and sacroiliac joint dysfunction.
3. Consequences of LLD
While the majority of LLD’s are clinically insignificant and silent, some significant or longstanding inequalities can contribute to a variety of conditions, including low back pain, scoliosis, and an increased risk of hip and knee osteoarthritis. (4-7)
4. Diagnostic Imaging for LLD
A December 2021 systematic review concluded that imaging was the most reliable and accurate mechanism to identify and quantify LLD. (8) Among the options:
Full-length standing anteroposterior radiography – “high-quality evidence that [this] is a valid method for determination of LLD […and is…] the global reference standard”.
Pelvic radiography with landmarks – “strong evidence, that validity of the pelvic radiography with pelvic landmarks is low.”
CT Scanogram – “moderate evidence, that the scanogram is reliable for measuring LLD.”
However, for most cases, many clinicians typically do not believe the risk: benefit ratio justifies LLD-specific imaging since:
Many LLD’s are clinically inconsequential.
Even when an LLD is relevant, the deficiency includes a combination of ever-changing functional contributors.
The imaging outcome will not often dictate the specific intervention (i.e., initial or ultimate heel lift height).
5. Clinical Assessment of LLD
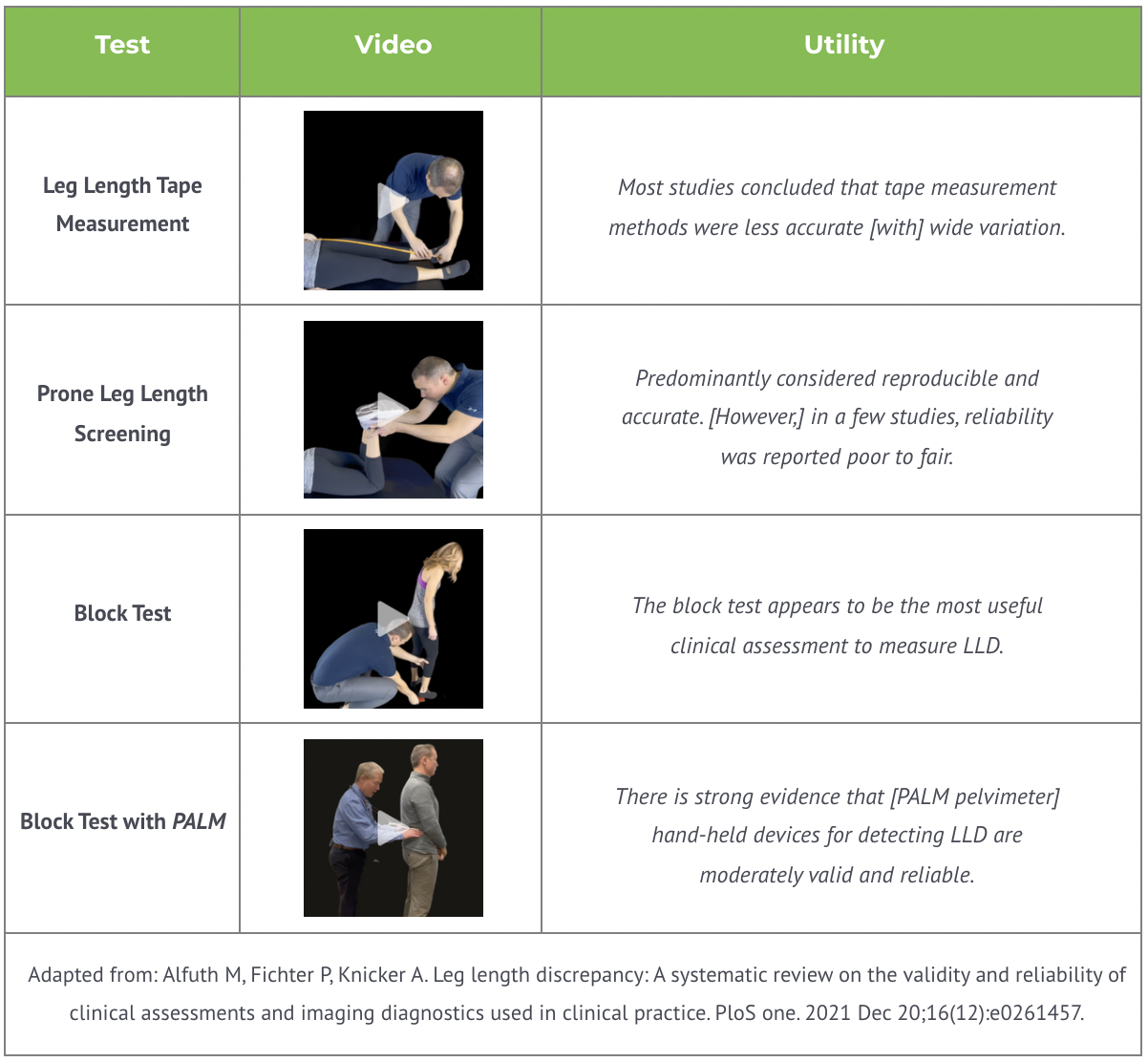
Alfuth’s systematic review of 37 articles on clinical assessments for LLD identified several non-invasive options, summarized in the following chart. (8)
6. Treatment threshold for LLD
Two 2020 studies highlight the ironic deficiency regarding leg length deficiencies:
“The evidence base on the indications for treatment of leg-length discrepancy is poor; only informal consensus recommendations are available.” (9)
“Leg length discrepancy (LLD) is a common condition. The threshold of LLD which is of clinical significance varies with studies, and there is at present no universal consensus.” (10)
The majority of patients exhibit some degree of LLD, and most adapt to the imbalance with no adverse effects. Unfortunately, some do not and will require intervention.
In the past, LLD’s > 6 mm were suspect. (11,12) More recent evidence suggests that up to 20 mm inequalities may not be significant. (1) Identifying which LLD’s require management is largely individual – as each patient is a case study of one. Many clinicians choose to address LLD’s only when symptoms persist and the patient has not responded to first-line correction of biomechanical and functional deficits (i.e., manual therapy and rehab).
7. Effectiveness of heel lifts for LLD
Correcting clinically significant LLD’s can impact outcomes. A 2019 study of symptomatic laborers with LLD’s concluded that incorporating insoles with heel lifts reduced the intensity of LBP (-2.6 average VAS improvement) and sciatica (-2.3 average VAS improvement), with significantly higher physical function and fewer sick days. (13)
8. Internal heel lifts vs. heel build-up for LLD
When a more significant heel lift is indicated, clinicians must determine how much of that lift can be placed inside the patient’s shoe before an external heel buildup is required. Considerations include shoe size, fit, and style (lace-up vs. slip-on).
Experts generally advocate internal lifts of up to 9 mm. (14-16). However, patients requiring more than 10 mm will likely require some external heel build-up from a qualified cobbler or shoemaker.
9. Introducing a heel lift
Many experts agree that heel lifts should be implemented gradually. (14) For small yet clinically significant LLD’s, clinicians can begin with a 1-3 mm lift, then gradually progress each week toward the target or until symptoms respond. To allow the body an opportunity to accommodate and respond, the build-up of larger discrepancies should generally not exceed 5-7 mm each month. (14)
10. The bottom line on LLD’s
The majority of patients exhibit some degree of LLD, and most adapt to the imbalance with no adverse effects. Unfortunately, some do not and will require intervention. Imaging is generally unnecessary. The block test with a PALM caliper inclinometer is a reliable non-invasive assessment and monitoring tool. When indicated, lifts should be implemented gradually until the desired clinical outcome is achieved.
Speaking of desired clinical outcomes…
We know that you strive day in and day out to give your patients the best possible care in order to achieve great outcomes. We are on the same mission as you. ChiroUp gives you clinical resources from the initial diagnosis to the patient’s release so that you can be confident delivering the highest standard of care for every patient, every time. Get started now!
-
Knutson GA. Anatomic and functional leg-length inequality: a review and recommendation for clinical decision-making. Part I, anatomic leg-length inequality: prevalence, magnitude, effects and clinical significance. Chiropractic & osteopathy. 2005 Dec;13(1):1-0. Link
Kayani B, Pietrzak J, Hossain FS, Konan S, Haddad FS. Prevention of limb length discrepancy in total hip arthroplasty. British Journal of Hospital Medicine. 2017 Jul 2;78(7):385-90. Link
Gurney B. Leg length discrepancy. Gait & posture. 2002 Apr 1;15(2):195-206. Link
Lewis CE, Felson DT. Association of Leg-Length Inequality With Knee Osteoarthritis. Ann Intern Med. 2010;152:287-95. Link
Tallroth K, Ristolainen L, Manninen M. Is a long leg a risk for hip or knee osteoarthritis? A 29-year follow-up study of 193 individuals. Acta orthopaedica. 2017 Sep 3;88(5):512-5. Link
Rannisto S, Okuloff A, Uitti J, Paananen M, Rannisto PH, Malmivaara A, Karppinen J. Leg-length discrepancy is associated with low back pain among those who must stand while working. BMC musculoskeletal disorders. 2015 Dec;16(1):1-7. Link
Campbell TM, Ghaedi BB, Ghogomu ET, Welch V. Shoe lifts for leg length discrepancy in adults with common painful musculoskeletal conditions: a systematic review of the literature. Archives of physical medicine and rehabilitation. 2018 May 1;99(5):981-93. Link
Alfuth M, Fichter P, Knicker A. Leg length discrepancy: A systematic review on the validity and reliability of clinical assessments and imaging diagnostics used in clinical practice. PloS one. 2021 Dec 20;16(12):e0261457. Link
Vogt B, Gosheger G, Wirth T, Horn J, Rödl R. Leg length discrepancy—treatment indications and strategies. Deutsches Ärzteblatt International. 2020 Jun;117(24):405. Link
Rothschild D, Ng SY, Ng YL. Indications of sole lift and foot orthoses in the management of mild idiopathic scoliosis—a review. Journal of physical therapy science. 2020;32(3):251-6. Link
Cyriax J. Textbook of Orthopedic Medicine Vol I, 5th Ed. London: Baillare, Tyndall and Cassell, 1969
Taillard W. Lumbar spine and leg length inequality. Acta orthopaedica Belgica. 1969;35(3):601-13. Link
Rannisto S, Okuloff A, Uitti J, Paananen M, Rannisto PH, Malmivaara A, Karppinen J. Correction of leg-length discrepancy among meat cutters with low back pain: a randomized controlled trial. BMC musculoskeletal disorders. 2019 Dec;20(1):1-9. Link
Leg length discrepancies and shoe lifts. The Gait Guys Blog. September 8, 2021 Accessed on 2/2/2022 from: https://www.thegaitguys.com/thedailyblog/leg-length-discrepancies-and-shoe-lifts
Michaud TC. Foot orthoses and other forms of conservative foot care. Williams & Wilkins; 1993.
Valmassey R. Clinical Biomechanics of the lower extremities. Mosby, St Louis, Philadelphia. 101-107: 1996