10 Clinical Pearls and One Very Useful Test for Groin Strain
Groin disorders comprise 2-5% of all athletic injuries. (1) Groin pain is particularly challenging considering its associated disability, high recurrence, and propensity toward lingering symptoms. (2) Strains involving the adductor muscles are the most common groin injury.
To simplify your job of managing groin strains, the ChiroUp advisory board has scoured the evidence-based literature and collaborated to create another “best practice” chiropractic protocol. Here are our top ten clinical pearls for Adductor Strains, including a video demonstration of a useful orthopedic test to help localize the site of groin injury.
1. While many clinicians regard limited abduction as a risk factor, several studies have found no relationship between adductor flexibility and groin strain. (3-5)
2. Athletes with a thigh adductor: abductor strength ratio of less than 4:5 are at higher risk of groin strain. (6-8)
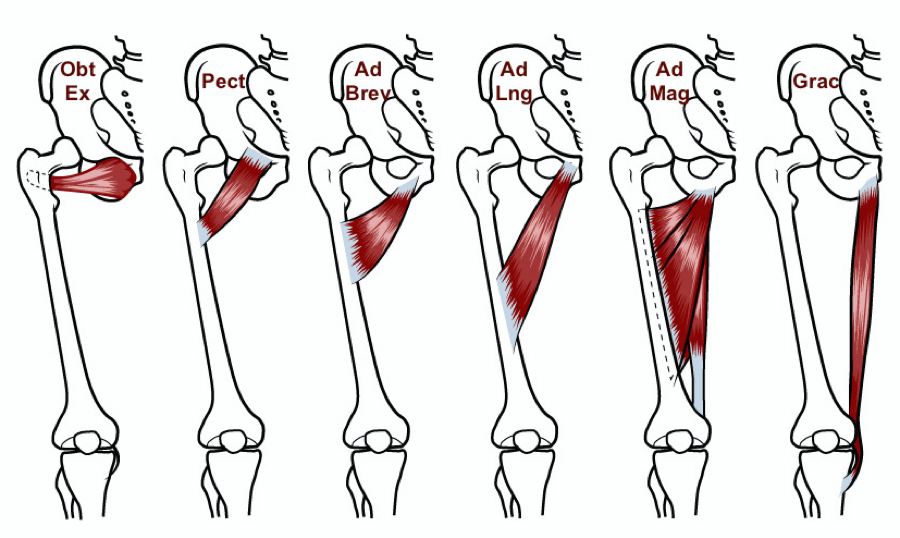
3. The adductor longus has a relative mechanical disadvantage for explosive actions that require the adductors to contract eccentrically; i.e., decelerate an abducted and extended thigh, and not surprisingly, is the most frequently strained adductor muscle. (9,10)
4. Acute groin strains generally involve the vulnerable musculotendinous junction or muscle belly, while chronic repetitive stress characteristically leads to more proximal irritation at the tendinous insertion, particularly in adolescents, i.e., apophysitis.(11,12)
5. The Thigh Adductor Squeeze Test is a reliable provocative orthopedic test where the supine patient forcefully adducts their thighs to compress a fist or ball placed between their knees. (13-15)
6. Adductor pain or weakness accompanied by sensory loss in the medial thigh could suggest obturator neuropathy, which sometimes masquerades as or accompanies groin strain. (16)
7. Exquisite tenderness over the pubic symphysis should raise suspicion for osteitis pubis (inflammation of the pubic symphysis). (17)
8. Reproduction of symptoms upon abdominal pressurization tests, including Valsalva or resisted sit up, suggests sports hernia (weakening and tearing of the posterior inguinal wall from the superior pubic ramus). (8)
9. While active treatment of bone-tendon injuries may necessitate delay until acute symptoms improve, tears involving the more vascularized musculotendinous junction or muscle belly can generally tolerate an earlier rehab. (18,19)
10. Biomechanical deficits involving the pubic symphysis or sacroiliac joints can inhibit the pelvis’s ability to transfer force leading to excess myofascial strain.
Subscribers can log on to ChiroUp.com to review the entire best practice protocol for groin strain - including the most sensitive tests and other valuable management suggestions. Then practice with confidence knowing that you are delivering the most appropriate exercises and ADL advice to your patients...automatically.
If you’re not yet a subscriber, click here to start your free trial today. No credit card, no commitment.
-
Morelli V, Smith V. Groin injuries in athletes. Am Fam Physician 2001 Oct 15;64(8):1405-14.
Delahunt E, Thorborg K, Khan KM, et al. Minimum reporting standards for clinical research on groin pain in athletes. Br J Sports Med 2015;49:775-781.
Emery CA, Meeuwisse WH, Powell JW. Groin and abdominal strain injuries in the National Hockey League. Clin J Sport Med. 1999;9(3):151-156
Emery CA, Meeuwisse WH. Risk factors for groin injuries in hockey. Med Sci Sports Exerc. 2001;33(9):1423-1433
Tegner Y, Lorentzon R. Ice hockey injuries: incidence, nature and causes. Br J Sports Med. 1991;25(2):87-89
Tyler TF. et al. Groin Injuries in Sports Medicine. Sports Health. 2010 May; 2(3): 231–236.
Crow JF, Pearce AJ, Veale JP, VanderWesthuizen D, Coburn PT, Pizzari T. Hip adductor muscle strength is reduced preceding and during the onset of groin pain in elite junior Australian football players. Journal of Sciences and Medicine in Sport 2010;13(2):202e4.
Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility on the incidence of groin strains in professional ice hockey players. Am J Sports Med. 2001;29(2):124-128
Davis JA, Stringer MD, Woodley SJ. New insights into the proximal tendons of adductor longus, adductor brevis and gracilis. Br J Sports Med 2012;46:876—971.
Norton‐old, Kimberley J., et al. Anatomical and mechanical relationship between the proximal attachment of adductor longus and the distal rectus sheath. Clinical Anatomy 26.4 (2013): 522-530.
Schilders EM. Groin injuries in athletes. Curr Orthop 2000;14:418—23.
Groin strain. (2017, September 28). Physiopedia. Retrieved December 12, 2017 from https://www.physio-pedia.com/index.php?title=Groin_strain&oldid=179346.
Verrall GM, Slavotinek JP, Barnes PG, Oakeshott RD, Spriggins AJ, Barnes PG, et al. Description of pain provocation tests used for the diagnosis of sports-related chronic groin pain: relationship of tests to defined clinical (pain and tender- ness) and MRI (pubic bone marrow oedema) criteria. Scandinavian Journal of Medicine and Science in Sports 2005;15(1):36e42.
Malliaras P, Hogan A, Nawrocki A, Crossley K, Schache A. Hip flexibility and strength measures: reliability and association with athletic groin pain. British Journal of Sports Medicine 2009;43(10):739e44.
Fulcher ML, Hanna CM, Raina Elley C. Reliability of handheld dynamometry in assessment of hip strength in adult male football players. Journal of Science and Medicine in Sport 2009;13(1):80e4.
Bouvard M, Lippa A, Reboul G, Lutz C. La pubalgie du sportif. J Traumatol Sport 2012;29:105—28.
Charles Andrew. 69: Athletic Pubalgia Gilliland Clinical Orthopaedic Rehabilitation: a Team Approach (Fourth Edition), 2018, Pages 462-465.e1
Fricker PA. Management of groin pain in athletes. Br J Sports Med. 1997;31:97–101.
O’Connell MJ, Powell T, McCaffrey NM, O’Connell D, Eustace SJ. Symphyseal cleft injection in the diagnosis and treatment of osteitis pubis in athletes. AJR Am J Roentgenol. 2002;179:955-959.