Chiropractic Management of Compression Fractures
Previous blog: 5/20/2021
Reading time: 5 minutes
Effective and efficient chiropractors ask the right questions, allowing them to perform the most sensitive orthopedic testing to identify damaged tissue. Unfortunately, some pain generators within the spine are elusive to traditional orthopedic testing and history taking. This blog will dive deeply into one of the most common types of pain generators: vertebral fractures.
These pesky structural changes may limit your clinical effectiveness and patient satisfaction. The following information will cover the essentials of recognizing vertebral fractures, when to refer out, and arm you with proper patient education for those patients considering surgical intervention.
Did You Know?
“Approximately 80% of patients experience at least one unnoticed vertebral compression fracture (VF) before being eventually diagnosed. Only 1/3 of patients with VFs seek medical attention due to spinal pain, while the rate of misdiagnosis is up to 40% at the point of care." (1)
There are two main types of compression fractures:
1. Endplate Fracture
2. Vertebral Compression Fracture
Endplate Fractures
Minor compression fractures of the vertebral endplate are called Schmorl’s nodes. Historically, these are considered non-provocative for symptoms. However, Otaki et al. 2021 found a correlation between vertebral endplate changes and neck pain. This study of 582 cervical MRIs indicated one variable associated with neck pain. It wasn't degeneration of the disk or the surrounding bony structures. Instead, it was the presence of Schmorl’s nodes! (2)
What is a Schmorl’s node?
A Schmorl’s node is an INTRAvertebral disc herniation. Trauma or degeneration of the vertebral endplate results in a protrusion of the intervertebral disc (IVD) through the vertebral body endplate into the adjacent vertebra.
These protrusions result in:
Compression to the marrow of the adjacent vertebra causes inflammation. Surrounding bone marrow edema may be visualized upon advanced imaging. (3)
Loss of disc pressure and intervertebral stability
What happens to a disc with an endplate fracture?
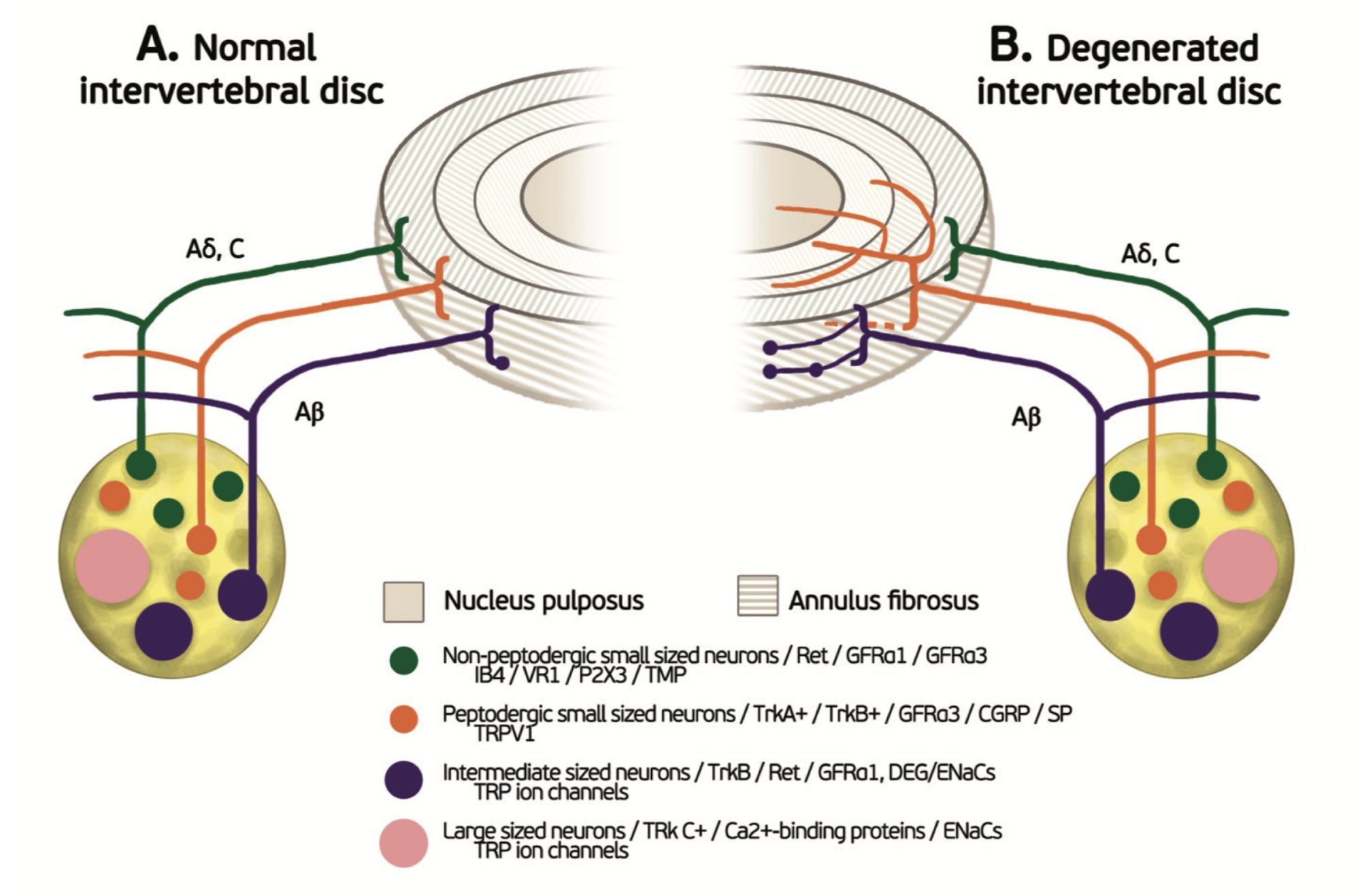
The superficial 1/3 of annulus fibrosis contains nerve fibers. Most nerve fibers within these layers are nociceptors (orange and green). However, some mechanoreceptors (purple) populate these layers for proprioception. After endplate damage, the IVD will begin to degenerate due to the loss of fluid and pressure. Both nerve fibers will begin infiltrating the annulus fibrosis and eventually the nucleus pulposus. Nociceptor and Mechanoreceptor density will also increase within the superficial layers of the annulus. (4)
So… Intravertral disc herniations are COMMON and can be SYMPTOMATIC?
Compression Fractures
In seniors, increased thoracic kyphosis or loss of lumbar lordosis should raise suspicion for VF. Multiple VFs can lead to a noticeable overall loss of height. There is a high incidence of compression fractures in elderly patients whose fingertips extend to the lower thigh when standing. Never miss a compression fracture again using these four tests:
1. The Back Pain-Inducing Test (BPIT)
Patients completed three consecutive movements (without any help) in the following order.
First, sitting on the table with legs dangling off the edge of the table, and then lying down in the supine position (lying supine);
Second, changing from the supine position to the left or right decubitus position with legs flexed, and then back to the supine position (rolling over);
Third, changing from the supine position to a sitting posture with the legs still on the bed (sitting up).
Back pain induced by any of these movements was documented using a patient-reported numerical rating scale (NRS). The following BPIT results were defined as positive:
Patients reporting back pain occurring during any movement or
Patients not being able to perform any of the three movements due to back pain.
Otherwise, the test results were deemed negative. (1)
2. Supine Sign
The inability to lie supine on an exam table with only one pillow supporting the head has a relatively high sensitivity (81%) and specificity (93%) for vertebral compression fracture.
3. Seated Closed Fist Percussion
Percussion of the spine has a sensitivity and specificity near 90% for vertebral compression fracture. Acute or "active" VF will likely limit the spinal range of motion.
4. Heel Drop Test
The Heel Drop Test may increase pain originating from VF. The presence of radicular complaints or neurological findings mandates further workup to evaluate the stability of the injury.
Osteoporotic vertebral compression fractures (OVCF) are twice as common as hip fractures. Clinicians should consider orthopedic referral for patients with radicular complaints attributable to VF. The presence of cauda equina symptoms (loss of bowel or bladder control, impotence, etc.) requires an immediate emergency referral.
Vertebral Fracture Patient Education
Is your patient considering invasive treatment? Educate them with the facts concerning vertebral augmentation strategies, i.e., vertebroplasty, and kyphoplasty.
One systematic review demonstrated that compared to patients choosing conservative therapy, OVCF patients undergoing percutaneous vertebroplasty demonstrated greater pain relief up to 1 year postoperatively. (5)
Many other vertebroplasty studies have failed to show significantly better long-term outcomes compared with conservative care. (6,7)
Guidelines recommend that patients with stable OVCF complete 3-4 weeks of conservative care before considering cement augmentation. (8-10)
Progressive increase in the fracture angle (>10 degrees) and persistent, progressive or debilitating pain may indicate earlier operative management. (11,12)
Studies concerning balloon kyphoplasty fail to support superiority over conservative care. (13-19)
ChiroUp subscribers can relay pertinent information to their patients in seconds with a condition report for Osteoporotic Vertebral Compression Fracture. If you aren’t a ChiroUp subscriber, there is no better time than now to sign up! Get started now!
-
Jin H, Ma X, Liu Y, et al. Back Pain-Inducing Test, a Novel and Sensitive Screening Test for Painful Osteoporotic Vertebral Fractures: A Prospective Clinical Study. J Bone Miner Res. 2020;35(3):488‐ doi:10.1002/jbmr.3912 Link
Otaki H, Otani K, Watanabe T, Sekiguchi M, Konno SI. Associations between clinical neck symptoms and various evaluations of cervical intervertebral disc degeneration by magnetic resonance imaging. Fukushima journal of medical science. 2021.
Diehn F, Maus T, Morris J et al. Uncommon Manifestations of Intervertebral Disk Pathologic Conditions. Radiographics. 2016;36(3):801-23.
K.A. Tomaszewski. et al. The biology behind the human intervertebral disc and its endplates. Folia Morphol. Vol. 74, No. 2, pp. 157–168
Mattie R, Laimi K, Yu S, Saltychev M. Comparing percutaneous vertebroplasty and conservative therapy for treating osteoporotic compression fractures in the thoracic and lumbar spine: a systematic review and meta-analysis. JBJS. 2016 Jun 15;98(12):1041-51. Link
Kallmes DF, Comstock BA, Heagerty PJ, Turner JA, Wilson DJ, Diamond TH, Edwards R, Gray LA, Stout L, Owen S, Hollingworth W. A randomized trial of vertebroplasty for osteoporotic spinal fractures. New England Journal of Medicine. 2009 Aug 6;361(6):569-79. Link
Buchbinder R, Osborne RH, Ebeling PR, Wark JD, Mitchell P, Wriedt C, Graves S, Staples MP, Murphy B. A randomized trial of vertebroplasty for painful osteoporotic vertebral fractures. New England Journal of Medicine. 2009 Aug 6;361(6):557-68. Link
Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, Venmans A, van Rooij WJ, Schoemaker MC, Juttmann JR, Lo TH. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. The Lancet. 2010 Sep 25;376(9746):1085-92. Link
Lee HM, Park SY, Lee SH, Suh SW, Hong JY. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): conservative treatment versus balloon kyphoplasty. The Spine Journal. 2012 Nov 1;12(11):998-1005. Link
Kaczynski J, Jakimiuk A. Vertebral fractures: a hidden problem of osteoporosis. Med Sci Monit. 2001;7(5):1108-7. Link
Mehta JS, Reed MR, McVie JL, Sanderson PL. Weight-bearing radiographs in thoracolumbar fractures: do they influence management?. Spine. 2004 Mar 1;29(5):564-7. Link
Gibson L. The mechanical behaviour of cancellous bone. Journal of biomechanics. 1985 Jan 1;18(5):317-28. Link
Liu JT, Liao WJ, Tan WC, Lee JK, Liu CH, Chen YH, Lin TB. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporosis international. 2010 Feb 1;21(2):359-64. Link
Yang H, Wang G, Liu J, et al. Balloon kyphoplasty in the treatment of osteoporotic vertebral compression fracture nonunion. Orthopedics 2010;33:24.
Dixon RG, Mathis JM. Vertebroplasty and kyphoplasty: rapid pain relief for vertebral compression fractures. Current osteoporosis reports. 2004 Dec 1;2(4):111-5. Link
Mathis JM, Ortiz AO, Zoarski GH. Vertebroplasty versus kyphoplasty: a comparison and contrast. AJNR Am J Neuroradiol 2004;25:840–5.
Chen JK, Lee HM, Shih JT, Hung ST. Combined extraforaminal and intradiscal cement leakage following percutaneous vertebroplasty. Spine. 2007 May 20;32(12):E358-62. Link
Park SY, Modi HN, Suh SW, Hong JY, Noh W, Yang JH. Epidural cement leakage through pedicle violation after balloon kyphoplasty causing paraparesis in osteoporotic vertebral compression fractures-a report of two cases. Journal of orthopaedic surgery and research. 2010 Dec;5(1):54. Link
Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. The Journal of bone and joint surgery. British volume. 2012 Feb;94(2):152-7.